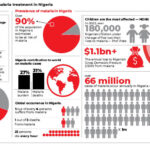
As the COVID-19 pandemic swept across the world this year, it brought challenges for people living with HIV/AIDs, and HIV response in the country. Months into the pandemic, people living with the disease and experts narrate how they were affected as well as their efforts to mitigate the impact.
Hannah, 45, could not get one of her antiretroviral drugs at the public hospitals in the state she lives in April.
She was told she could get it in Abuja. However, she couldn’t travel immediately because the federal government had imposed a lockdown in the Federal Capital Territory (FCT), Lagos, and Ogun states.
She decided to wait for the ease of lockdown even though she felt unwell. When the lockdown was eased, she discovered she couldn’t still travel because of the interstate travel ban. She grew increasingly ill as the days turned to weeks. Finally, she decided to brace it up and travel in early June.
“It was a harrowing experience. The journey took longer, especially coming to Abuja because of the many security check points,” she told Daily Trust.
Salami Idris (Not his real name) who is on third-line drugs on his part said he couldn’t access his drugs for several months because the COVID-19 pandemic caused disruptions in the procurement of such drugs by the country.
The National Coordinator of the Network of People Living with HIV/AIDS (NEPHWAN), Abdulkadir Ibrahim, said one reason the impact of the COVID-19 pandemic was felt by people living with HIV/AIDS was that majority of partners on HIV response were diverting resources from HIV to COVID-19, thereby leaving them with some issues that needed utmost attention.
“However, we are appealing to the whole world on the synergy between COVID-19 and HIV. Responding to COVID-19 should not take away the resources that are meant to take care of people living with HIV/AIDS,” he said.
According to him, many people living with HIV suffered during the lockdown as they were unable to access treatment at the due time.
The NEPHWAN national coordinator said as a result of stigma, some people living with the disease prefer to access treatment from faraway places and not where they live.
“For instance, someone living in Sokoto can go to Lagos or Abuja to get drugs but because of the lockdown, they couldn’t get treatment and this affected service uptake.”
He said to mitigate the impact in this area, his association used volunteers to make delivery at the community level.
Ibrahim also said there was a shortage in the global supply chain of HIV drugs before the advent of COVID-19 but the COVID-19 made it worse.
He added that it also affected production of drugs especially those on the second line, as the drugs were used for COVID-19 clinical trials.
“A lot of trials were ongoing on what could treat COVID-19. So a lot of our drugs were used before we raised alarm to the PTF on COVID-19, and the PTF coordinator intervened and gave instructions that such drugs should not be diverted from people living with HIV/AIDS,” he said.
Director-General of the National Agency for the Control of AIDS (NACA), Dr Gambo Aliyu, said COVID-19 caused some setbacks in HIV services but that the response in the country is back on track.
He said, “During the lockdown, we were not able to hold clinics, patients were not able to access medications, and some of the facilities were converted to isolation centres for COVID-19.”
Dr Aliyu said laboratories were also overwhelmed and the agency had to create a mechanism where staff worked during the day for HIV and ran tests for COVID-19 samples at night.
He said, “The good thing is at the time COVID-19 struck, Nigeria had a system in place to respond, and that platform was provided by HIV structures nationwide.
“We had labs that were ready to test, personnel that were trained and equipped to do the test and health workers that were deployed with hands-on training to stand up to the challenge.
“We also had volunteers at the community level that were very efficient in working at the community to message to the grassroots in supporting the response.”
The NACA DG said the country lost about half of the people it was supposed to identify and test for HIV as a result of the COVID-19 pandemic.
“It denied us the opportunity to identify several thousands of individuals over the period that would have been identified, and linked to care . So our trajectory clearly went down.

However, he added that following the relaxation of the lockdown, reduction in cases, and improvement in availability of personal hygiene and protective equipment, HIV response is back in full swing.
“We are doing tests and most of the facilities that were locked and converted to COVID-19 isolation centres are now back. Medications are also available. So our trajectories are now back to where we expect them, which means we are now where we expected to be in terms of our monthly identification of individual target that we expect to identify every month, and the target we expect to link to care every month,” he added.
Chief Executive Officer of the Institute of Human Virology Nigeria (IHVN), Dr. Patrick Dakum said HIV programmes in the country were affected by shortage of drugs, inability of patients to meet appointments, and conversion of facilities to isolation centres as a result of the pandemic.
He said, “First of all, HIV is a chronic infectious disease that requires lifelong treatment and people come periodically, either two monthly, or three monthly to collect their drugs when they are doing well. Remember that part of the measures taken to curb the spread of COVID-19 was the lockdown.
“Therefore, we had two kinds of barriers; the first barrier was that patients were locked down and could not go to the health facility to collect the drugs. Workers only started working on essential duties and a number of facilities were closed. There were also challenges of personal protective equipment (PPE) for health workers.”
He said new cases dropped, retention in care dropped, and monitoring for patients like viral load also reduced.
Dr Dakum said as implementing partners in the HIV response in the country, IHVN had to take measures to mitigate the impact. He added that now most of the HIV facilities are open and patients can get their drugs and get monitored.
“One of the measures that we took at the peak of the pandemic was decentralising the collection of drugs to either pharmacies or health care centres closer to where people are. They could walk in and as long as they present their hospital cards, they can get their refill for their drugs,” he said.
Other measures include using community workers to take drugs to those that could not go out at all, and leveraging the COVID-19 testing teams in communities to test for HIV, among others.
The NACA boss, Dr Gambo Aliyu, said the agency also developed innovations to ensure delivery of prescriptions and month-to-month refill.
He said another mitigating measure was communicating with people living with HIV AIDS in Nigeria on the measures they needed to take to protect themselves and stay COVID-19 free.
“One thing that we didn’t know in the past and we came to know is that HIV infected individuals are more likely to suffer negative consequences of COVID-19. They are two times more likely to die from COVID-19 than individuals that don’t have HIV,” he said.
According to him, measures by the agency to support the COVID-19 response in the country include sensitisation of the populace, providing laboratories, and supporting the PTF, Nigeria Centre for Disease Control (NCDC), and the Federal Ministry of Health in whatever way they could.
Also, the International AIDS Society (IAS) in a report it released during the 23rd International AIDS Conference entitled: COVID-19 and HIV: A Tale of Two Pandemics, noted widespread service disruptions, and provided two sets of recommendations for policymakers, healthcare providers, researchers, scientists, healthcare workers, communities and funders.
The first set of recommendations addressed HIV service delivery in the context of COVID-19, including shortening the length of health care visits and extending medication refills. The second set of recommendations addressed lessons from the HIV pandemic that could inform the COVID-19 response and this includes addressing social justice issues in the health care system and proactively addressing stigma.
WHO Director-General, Dr Tedros Adhanom Ghebreyesus, had during the conference shared findings of a WHO survey showing significant disruptions in access to HIV treatment.
On the theme of this year’s World AIDs Day, “Global Solidarity, shared responsibility,” the National Coordinator of the Network of People Living with HIV/AIDS (NEPHWAN), Abdulkadir Ibrahim, called for consistency in support for HIV response. He enjoined people living with the disease to also take responsibility by playing their own roles in preventing and minimising the risk of transmission, adhering to their drugs and also encouraging people to get tested.
“So we should unite against HIV/AIDS even with COVID-19. Our people should also to take responsibility by disclosing their HIV status to their family and loved ones so that they can live freely within their community and also get support and access drugs,” he said.

 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.