People infected with COVID-19 experience a wide range of symptoms and severities, the most commonly reported including high fevers and respiratory problems.
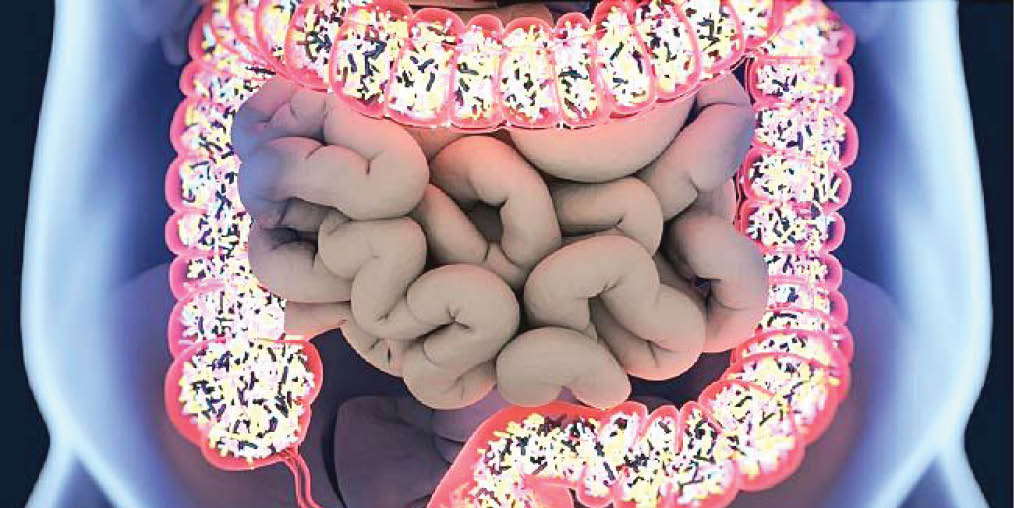
However, autopsy and other studies have also revealed that the infection can affect the liver, kidney, heart, spleen–and even the gastrointestinal tract.
- How strike, COVID-19 wrecked education calendar
- FCE Odugbo: Buhari’s magnanimity and Echono’s place of pride
A sizeable fraction of patients hospitalized with breathing problems also have diarrhoea, nausea and vomiting, suggesting that when the virus does get involved in the GI tract it increases the severity of the disease.
In a review published this week in mBio, microbiologist Heenam Stanley Kim, Ph.D, from Korea University’s Laboratory for Human-Microbial Interactions, in Seoul, examined emerging evidence suggesting that poor gut health adversely affects COVID-19 prognosis.
Based on his analysis, Kim proposed that gut dysfunction–and its associated leaky gut–may exacerbate the severity of infection by enabling the virus to access the surface of the digestive tract and internal organs. These organs are vulnerable to infection because they have widespread ACE2–a protein target of SARS-CoV-2–on the surface.
“There seems to be a clear connection between the altered gut microbiome and severe COVID-19,” Kim said.
Studies have demonstrated that people with underlying medical conditions including high blood pressure, diabetes and obesity face a higher risk of severe COVID-19. Risk also increases with age, with older adults most vulnerable to the most serious complications and likelihood of hospitalization.
But both of these factors–advanced age and chronic conditions–have a well-known association with an altered gut microbiota. This imbalance can affect gut barrier integrity, Kim noted, which can allow pathogens and pathobionts easier access to cells in the intestinal lining.
So far, the link between gut health and COVID-19 prognosis hasn’t been empirically demonstrated, Kim noted. Some researchers have argued, he said, that unhealthy gut microbiomes may be an underlying reason for why some people have such severe infections.
What studies have been done hint at a complicated relationship. A study on symptomatic COVID-19 patients in Singapore, for example, found that about half had a detectable level of the coronavirus in faecal tests–but only about half of those experienced GI symptoms.
That study suggests that even if SARS-CoV-2 reaches the GI tract, it may not cause problems. Kim also noted that a person’s gut health at the time of infection may be critical for symptom development.
Many recent studies have found reduced bacterial diversity in gut samples collected from COVID-19 patients, compared to samples from healthy people. The disease has also been linked to a depletion of beneficial bacterial species – and the enrichment of pathogenic ones. A similar imbalance has been associated with influenza A infection, though the 2 viruses differ in how they change the overall microbial composition.
The depleted bacterial species associated with COVID-19 infection include some families that are responsible for producing butyrate, a short-chain fatty acid, which plays a pivotal role in gut health by reinforcing gut-barrier function.
Kim said he started analyzing the studies after realizing that wealthy countries with a good medical infrastructure–including the United States and nations in Western Europe–were among the hardest hit by the virus. The “western diet” that’s common in these countries is low in fiber, and “a fibre-deficient diet is one of the main causes of altered gut microbiomes,” he said, “and such gut microbiome dysbiosis leads to chronic diseases.”
The pathogenesis of COVID-19 is still not fully understood. If future studies do show that gut health affects COVID-19 prognosis, Kim argued, then clinicians and researchers should exploit that connection for better strategies aimed at preventing and managing the disease. Eating more fibre, he said, may lower a person’s risk of serious disease. And faecal microbiota transplantation might be a treatment worth considering for patients with the worst cases of COVID-19.
The problem with gut health goes beyond COVID-19, though, he said. Once the pandemic passes, the world will still have to reckon with chronic diseases and other problems associated with poor gut health.
“The whole world is suffering from this COVID-19 pandemic,” Kim said, “but what people do not realize is that the pandemic of damaged gut microbiomes is far more serious now.”
Courtesy: eureka
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


