Monitors under the auspices of the Public Private Development Centre found health centres under staffed or dilapidated and store loads of expired medicines.
Some health centres were completely unused were so remote it took almost three hours through rough terrain for locals to locate them, the monitors said.
“In almost all I visited, there was no drinking water,” said Anene Ekene, a monitor who visited health centres in Lere and Kudau local government areas of Kaduna state. “They shotput [defecated in polythene bags to be thrown away].”
“In one of them I entered, almost all the drugs had expired. I asked why the drugs weren’t given out and was told nobody came for them,” said Ekene. “So why not discard them? Anybody who comes to help, when they see these drugs, they will feel like there are drugs.”
At one site the building for the health centre had “fallen to the ground” and work was replicated to a room in the home of the village chief, a mud hut where community health extension workers treat children, he added.
“Access to road is something else. We had to enter a bush and be there for two, three hours trying to locate one or two health centres,” said Ekene.
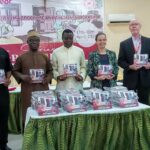
The visits to monitor primary health centres came after PPDC put up a Freedom of Information request to the National Primary Health Care Development Agency, which coordinates primary health care across the country.
The agency responded with a list of recently built centres, with up to a thousand across the three states.
“It was a very long list, and it looked like every year primary health centres were being built,” said Seemed Nyager, director of PPDC.
“And we wanted to know what kind of service was actually been attained in those places. We asked for minimum-care standards because we wanted to know what kind of services people can access in those places.”
In Chikun and Igabi local government areas of Kaduna, Obinna Ezeaku acted as a patient and was impressed with the response of health workers, he reported.
But many centres had a single toilet for both males and females. “None had water and they were complaining bitterly because of the distances they have to walk.”
Victoria Onyeacho, who went to Kagarko, Jiba, Kajuru and Kauru local government areas of Kaduna found a lack of toilets and water to maintain sanitation and hygiene.
She also found many health centres deserted or closed.
“The matrons come from afar, get there by ten, close work by two to go back home. Mostly they [visited community residents at] home. And if the case is serious, they refer them to the general hospital,” said Onyeacho.
PPDC used the minimum-care standards provided by NPHCDA to develop a checklist on which monitors ticked off equipment and services at the random health centres.
In Doma and Lafia local government areas of Nasarawa Udochi Eze found health willingly listing what they lacked and what any partnership could afford them.
“They said they needed help,” Eze said. “Some of the primary health centres were mud houses and badly ventilated. Most don’t have access to good water and roads. And security is a major issue both in Lafia and Doma. This Fulani-herdsmen clash with local communities is really affecting their primary health centres there.”
Chinyere Nkwo found an ideal health centre in Kwali area council of the FCT. In another case, she rode on a bike for hours far into remote locations until “I was getting scared,” she said. “I finally got there and it was locked. Locals told me the health workers don’t really come there most of the time and they have gone to town.”
Areas like Kilankwa and Mongo had bad roads. “Most of the places, the bike operators don’t really like to go there. They say it is too far or they simply don’t want to go there.”
The monitors found wide differences between their checklist and the equipment and services available in health centres. Grading of primary health centres into types–as health post or dispensaries–which determine their capacity was inadequate.
Nyager called it “fundamentally wrong.” “People should know ahead of time that this sort of service is not done in this kind of place, because there is no point wasting time going there she you know you won’t get a particular service,” she said.
The assessments are still ongoing and will get to mother states. PPDC is still analyzing reports from its monitors and wants to take its final findings to authorities to advocate better health care at rural levels where residents’ only access to care is at primary health centres.