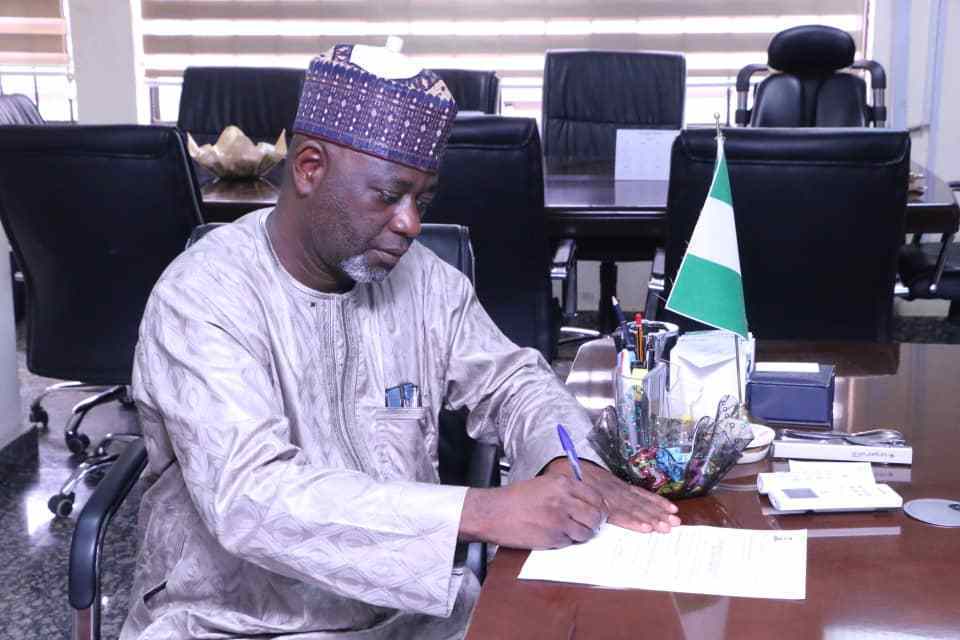
In this interview, Professor Mohammed Nasir Sambo, the executive secretary of the National Health Insurance Scheme (NHIS), spoke on health insurance coverage for Nigerians, decentralisation of work and professionalism in the organisation, among other issues.
There have been calls to include care for cancer, kidney and other chronic diseases in the National Health Insurance Scheme. What are you doing about that?
The inclusion of cancer is one of the topical issues in the scheme. We have been able to develop a document called Essential Services and Drug List under the NHIS. We developed that document and put it on our website because of the concern that people are not aware of it.
If you browse the NHIS website and the document you would see that some level of drugs and intervention for the diseases are included in the benefit package.
However, comprehensive treatment of cancer is capital intensive. The health insurance here has been contributory, and the salaries of the people determine how much is contributed.
If the salary level is not good, you will not be able to cover a lot. So in countries where they recognise this, chronic diseases are usually handled by the government through the Federal Ministry of Health.
But since there are calls for the inclusion of cancer in the NHIS, we are discussing with the Federal Ministry of Health and other stakeholders to see how a fund that would be called ‘catastrophic fund for cancer’ will be established.
Some international partners have indicated willingness to support, so that we can have a dedicated fund for cancer, and enrollees with cancer can then get comprehensive care for the disease.
Before your appointment, the organisation was enmeshed in crises because of the issues between your predecessor and the immediate past minister of health. What is your relationship with the present minister?
In any system that is organized, there is hierarchy, command and subordination. The law establishing the organisation is very clear on what the role of the minister is and that of the head of parastatal or chief executive officer.
A chief executive officer of a parastatal is supposed to be subordinate to the minister. So if you hear any quarrel between them it means someone is infringing into somebody’s domain. If there is a particular issue that will require ministerial consent and I decide to hold it within the organisation, then there is a problem. This kind of thing will not happen under my stewardship.
The minister, Dr Osagie Ehanire, is a person that will not infringe in a domain or parastatal; similarly, myself as a professor of health policy and management, who has worked in a public system and in academia, I don’t think I should have cause to have any quarrel with my superior officers.
I will control what is within my purview. As a result of this, things have been working perfectly, not only between me and the minister of health but other stakeholders that are working within the NHIS.
What have you been doing to reposition the organisation since you took over in 2019 to fast-track access to health care for Nigerians?
Because the Scheme has passed through serious turbulence, there is, therefore, the need to rebrand it. So in the last 20 months, I have been rebranding it.
The Scheme has battled with excesses of Health Maintenance Organisations (HMOs) over the years. How are you addressing the problem?
There have been so many bottlenecks that hampered the smooth operation of the NHIS like enrollees being denied care. And when we dug deep, we discovered that the monetary payment system was replete with a lot of delays.
There was delay within the value chain of money transmission between the NHIS and HMOs, and between HMOS and health providers.
We have restructured our payment structure to HMOS to be on a quarterly basis. So with this, the NHIS no more delays payment. The HMOs now pay facilities without delay.
So we have been able to control the situation of enrollees being denied access to care on account of delay in payment or non-payment of their own contribution to the healthcare facilities.
We are also looking at the issue of drug supply. A lot of enrollees complain that the drugs they receive under the NHIS are fake and substandard. The NHIS drug list, which is in tandem with the national drug list, usually comes in generic and not branded forms.
We have had a series of discussions with drug manufacturers, with the view of producing drugs with NHIS inscription, so that wherever you go and get the drug as an enrollee, you know it is not fake or substandard. This is coupled with the enlightenment we are doing.
Our people should know that the generic name is the scientific name of the drug while branded drug is the copyright of a particular company.
What mechanisms have you put in place for recalcitrant HMOs that are not keying into the new measures?
Every stakeholder in the NHIS must imbibe transparency and accountability. In line with this, HMOs must ensure prompt payment of healthcare facilities. And healthcare facilities must provide prompt and quality services to enrollees.
When we came in we discovered that HMOs were owing healthcare facilities billions of naira, so we placed an advertisement that any healthcare facility that is being owed by HMOs should submit application. We then began the process of decentralising coordination at the state level and brought HMOs and healthcare facilities and their claims together.
The exercise took two months and we were able to aggregate close to N5billion being owed by HMOs. In the process of reconciliation, we discovered that there were some funds out of that N5billion that were not controversial at all.
We were able to recover N2.3 billion for healthcare facilities from HMOs , and they were happy because some of these debts were as far back as seven years ago. Some of them had almost lost hope of getting their money.
From the reconciliations we have been able to delist 10 HMOs. That is the first time it is happening in the annals of the Scheme. It was not easy for me after delisting them because of the serious backlash. But because we are doing a national job, we knew it was going to be tough. We have to sanitise the system.
For the remaining money we have not been able to reconcile, we employed the services of independent forensic auditors who will go deep into the books to ascertain the claims.
After the forensic reconciliation, we will take legal action for any money not recovered. We have to take legal means to ensure that the HMOs pay the money, even if they are among the delisted ones.
What chaneges do you expect from the amendment of the NHIS Act?
The procedure of changing or drafting a bill involves comparing it with other bills to ensure there is no contradiction or overlap. So the people who initiated the amendment of the bill wanted to make it a National Health Insurance Commission, but the National Insurance Commission (NAICOM) is already in existence. In fact, if you inadvertently do not see the H in the National Health Insurance Commission you may mistake it for the NAICON.
So, when the NAICON made some observations on this, the legislators that spearheaded the amendment of the act took cognizance of it. Therefore, if assented to, the NHIS would be called National Health Insurance Authority, just as it is in Ghana. This is to ensure there is no overlap or contradiction.
What is the current health insurance coverage level for Nigerians?
At the last count, we have been able to cover 12million people in Nigeria, and the number is increasing.
What is the update on the presidential action plan?
The points that were handed over to us when we came in had 10 items. And the presidency expected us to address all the action points. I am happy to tell you that almost all of them have been addressed. The only thing we are waiting for, which is crucial, is for the president to assent to the amended mandatory bill, which is one of the points.
How has the COVID-19 pandemic affected the organisation?
The pandemic caused some setbacks, but we have been able to cope with the situation. We have been able to ensure that services for other ailments are not stopped.
The NHIS played a significant role at the initial stage of the COVID-19 pandemic. For instance, utilisation of healthcare facilities nosedived to almost zero level, but our quick intervention in giving quarterly payment helped to sustain them.
In addition, the NHIS, despite not being a supply agency, contributed in providing Personal Protective Equipment (PPEs) to a lot of healthcare facilities and institutions that are frontline in providing COVID-19 care.
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


