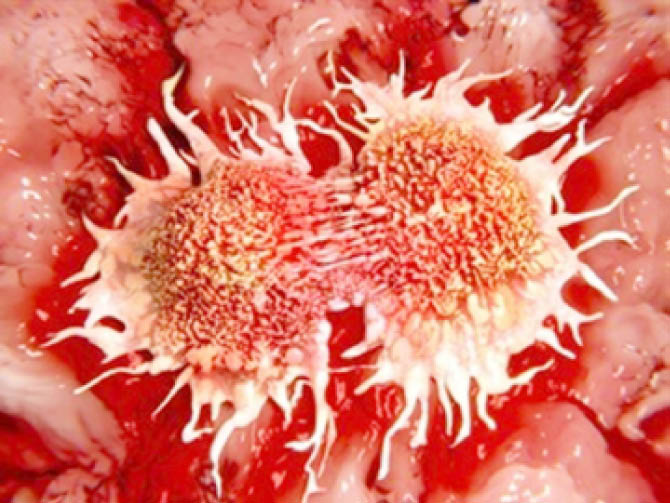
When cancer cells metastasize, they morph, becoming missile-shaped in order to penetrate into other tissues throughout the body.
In fact, to travel throughout the body, metastatic cancer cells must change their phenotypes-;their physical characteristics. This change allows stationary, epithelial cells which compose the barriers of our organs and our skin, to morph into mesenchymal cells, or the cells that develop into connective tissue, blood vessels and lymphatic tissue.
Researchers have observed that cells that complete this transition, called epithelial to mesenchymal transition, or EMT, can significantly increase the likelihood that a cancerous tumour will metastasize.
Currently, the way scientists screen and identify these cells is by observing them while fixed on microscope slides. But the standard studies looking at cells immobilized on microscope slides cannot reveal their shape shifting, no more than pinned butterfly collections can reveal their flight pattern, University of Michigan researchers write.
Now, the U-M researchers have developed a method to evaluate the cells while they are free to metamorphose, using a method called cell magneto-rotation as well as machine learning. Their results are published in the journal PLOS One.
To be able to observe these cell dynamics, the U-M researchers need the cell to be freely floating, rather than fixed on a glass slide. So they used their previously developed method-; cell magneto-rotation-; as the basis to study these cell dynamics.
Using this method and two well-known breast cancer cell lines that have different metastatic potential, Kopelman and colleagues load cancer cells into what’s called a microfluidic cell slide, composed of thousands of compartments. Each of the compartments holds only a single cancer cell.
Onto this slide, the researchers add a solution of commercially available magnetic nanoparticles. These nanoparticles enter the cancer cells but don’t cause harm to them. Then, a magnet rotates around the tray of cancer cells, which slowly rotates the cancer cells. The slow rotation does not affect the shape of the cell, but it does allow the cancer cell to shape-shift.
As the cells rotate, they are able to change their morphology similar to the way they would in the body. While they change the form, the researchers take fluorescent images of the cells. Then, they combine two algorithms-; object recognition and machine learning-; to identify each of the cells by its shape.
First, the researchers found that the cells that had undergone EMT were found to be shaped quite differently from the control population, demonstrating a strong relationship between a cell’s morphological and biological behaviours.
“This new machine learning-based method appears to have the potential to map and classify the morphodynamic distribution of a cell population, and thus to provide information on the degree of morphological plasticity of a tumour cell’s population, and such plasticity often correlates with lethality,” Kopelman said.
To analyze cells that go through significant changes in shape, the researchers forced a human prostate cancer cell line, PC-3, to go through the epithelial-to-mesenchymal transition. Using cell magneto-rotation, the researchers were able to identify not only the cells that underwent the transition but also the presence of even more subsets of the original cells.
Finally, they wanted to identify highly mobile cells within the population of breast cancer cells. They compared the images of these highly mobile cells to cells in the breast cancer lines that failed to migrate (using a standard test) and were able to distinguish the population of mobile cells from the general population of the breast cancer cells.
“What we hope is that this particular method will eventually be widely available and will give the treating doctor information on the aggressivity of specific cancer,” Kopelman said. “What we need are newer, better, additional tests to give caregivers additional information. I hope this microfluidic device will eventually be a standard option for screening cancer cells.”
Culled from https://www.news-medical.net
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.