Precious Chidinma Akpaduwa had been working up the guts to see a doctor but had other considerations: the hurdle of distance and time. Then she learnt she could book an appointment online and gave it a try.
She went online, downloaded an app, and signed up.
“The first thing was booking consultation with a doctor. I actually had a health need,” says Akpaduwa, a corporate worker and business owner.
“Before the time I was to do the consultation, I had been thinking of going to see a doctor, but because of the whole distance and time and everything, I couldn’t make it.”
- Ohanaeze to Tinubu: Halt persecution of Igbo in Lagos
- Oil price trades below $80 as EIA loses 3.8 million barrels
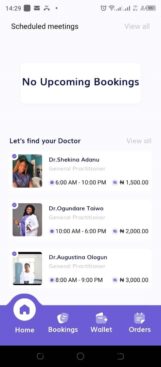
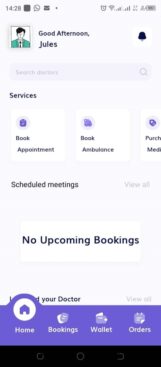
The app Rigour+ is using telemedicine to bring healthcare within reach of many in the country—and by extension cutting down patient waiting time by putting healthcare in the palm of users. Patient waiting time can last up two hours, according to some studies.
The app’s developers call it “redesigning the health space between patients and doctors” to change the way healthcare is accessed and delivered.
“Through virtual consultations, online pharmacy services, track-and-trace technologies, and an emergency response system, Rigour+ connects patients, doctors, pharmacies, and manufacturers seamlessly,” says Linda Obi, chief executive officer of Afri-Health, which developed the app.

“This comprehensive approach fosters better care coordination, improves patient outcomes, and reshapes the healthcare landscape, particularly in Nigeria and Africa, where fragmentation has been a longstanding issue.”
Many faces, one app
Nigerians are not new to health apps but telemedicine is still on the up in Nigeria. Policy regulations around it are still sketchy.
Rigour+ joins a handful of telemedicine apps already existing on app stores. It has taken four years of conception and creation before its launch this April. It has recorded over 7,000 downloads on Google Play Store alone and seen more than 900 patient-doctor consultations. Over 8,000 certified drugs have been onboarded and more than 500 pharmacies signed up to make medications available to users like Akpoduwa.
And at least 200 doctors have been verified and onboarded to provide consultation, and recruiters are scouting for more.
Benita Uzonwanne, a general practitioner, is among doctors fully onboarded—that means doctors with their licence and certifications verified before they can be visible to patients.
The number of consultations she gets depends on the number of patients using the app—10 in one week, 15 in another, 20 the next.
“The more patients that come online, the more consultations we get,” she explains.
So far, there’s been no barrier to the specialties that the platform can accommodate.
“Some specialties might not be able to use telemedicine because they may need to see the patient physically,” says Uzonwanne.
“What we are doing is getting as many specialties onboarded so that when patients come in, they can get at least a solution. If not a solution, then an immediate consult before they have to go to hospital later.”
“Imagine waiting two months to see a urologist because he is fully booked,” Uzonwanne explains.
“On the app, you don’t have to wait. Some [specialists] have their hospitals where they work. It is like giving you easy access to these doctors. If you see them online, they might proffer solutions right there, or if they think it is something you need to come in for, you have jumped the queue. They tell you, ‘all right, come to so-so-so hospital’. Again, this is verified, so there is no fear of things going sideways. They and the hospitals are verified. In this situation, you have saved months of time.”
Learning phases

Rigour+ is in its beta phase. Its alpha release was a time of insight and feedback from early users.
The importance of “intuitive user interface”, the lot of people that an ecosystem of an entire health care on an app could be life changing for, and the need for comprehensive user onboarding and support were all lessons in the alpha phase, said Afri-Health product manager Aderonke Babatunde.
“Additionally, we gained insights into the specific features and functionalities that resonated most with users, which helped shape our development roadmap for the beta phase.”
In the beta phase, developers look to resolve functional and user experience issues—to improve navigation, optimize performance and speed and refine appointment booking and processing orders of medication purchase.
Digital is the future, and so there is hope for almost any solution. An optimal success for Rigour+ is widespread impact across Nigeria to bridge healthcare gap in “underserved regions” and to set a precedent for “healthcare transformation” in Africa, says Obi.
“This entails joining hands with state and federal governments to amplify our efforts at scale, ensuring equitable access to quality healthcare for all.
“A significant milestone would be crossing 10 million downloads, with even a 1% conversion rate, signifying the successful adoption and utilization of our platform by millions of users.”
Horizons to push
Challenges lay ahead as well. Rigour+ is not alone in the telemedicine space attempting to bring healthcare to users on an app in the comfort of their homes.
CribMD, Tremendoc, DRO Health, Health Connect 24/7 and Doctall are only a start. Hudibia, Doctorcare247, LaFiya Telehealth and Reliance HMO are also among telemedicine apps competing for the attention of users on both different existing mobile platforms and app stores—all getting favourable ratings and reviews on a number of bases.
“It’s important to note that the digital health space is dynamic, and new entrants or existing players may emerge as competitors,” says Babatunde.
“We closely monitor the industry landscape and continuously strive to enhance our offerings to stay ahead of the competition.”
And that means using feedback to fix issues flagged by users. One complained of a booked appointment timing out and raised concern with reviewing refund policy.
“In this case, the doctor didn’t respond to the request until it was late and we understand how frustrating this can be to the user so we took that feedback and implemented an automatic time-out feature that cancels the request and notifies the user when the request has spent a certain amount of time with no response from the doctor,” Babatunde says in response to the review.
“We are also reviewing our refund policy to ensure it adequately addresses cases where appointments are canceled by either party.
“We do our best to ensure that all doctors are readily available to take appointments and we regularly send reminders and notifications to both the users and the doctors throughout the process.”
Akpaduwa noticed the improved feature on her subsequent use of the app.
Another user, Benedict, wanted more—a feature that allows users while video conferencing in a public space to drop discretely slide in a direct in-chat message when speaking out loud would be terrible for privacy.
He had consultation on the app until he got his prescription.
“My appointment [with the doctor] was successful,” he says. “I’m seeing the result in the medication I’m taking.”
The seamless link means he was able to get consultation, referral, laboratory tests, prescription and his drugs all on a single portal. But that draw of telemedicine comes with several limitations outside of the control of apps and their developers.
Ensuring reliable internet connectivity for virtual consultations, managing emergency cases that may require in-person medical attention, ensuring data privacy and security, and addressing potential disparities in access to technology among certain populations are just a few Obi envisages.
Another notable limitation is the complex regulatory environment that governs healthcare technology, requiring thorough compliance and adherence to data privacy and security regulations, says Babatunde.
Another is the interoperability of healthcare systems and integration with existing infrastructure can pose challenges.
“The critical lesson learned is the importance of close collaboration with healthcare stakeholders, including healthcare providers, regulatory bodies, and policymakers, to ensure seamless integration and effective implementation,” she adds.
Getting all that in place would provide an optimum experience for Akpaduwa, no waiting time, an entire health care ecosystem, right in her palm.
“You don’t have to stress yourself going to look for a hospital to see a doctor,” she says.
“And the stress of waiting on the queue is another thing that most people don’t like.”
This story was produced in partnership with Nigeria Health Watch through the Solutions Journalism Network, a non-profit organisation dedicated to rigorous and compelling reporting about responses to social problems.

 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


