By Ojoma Akor
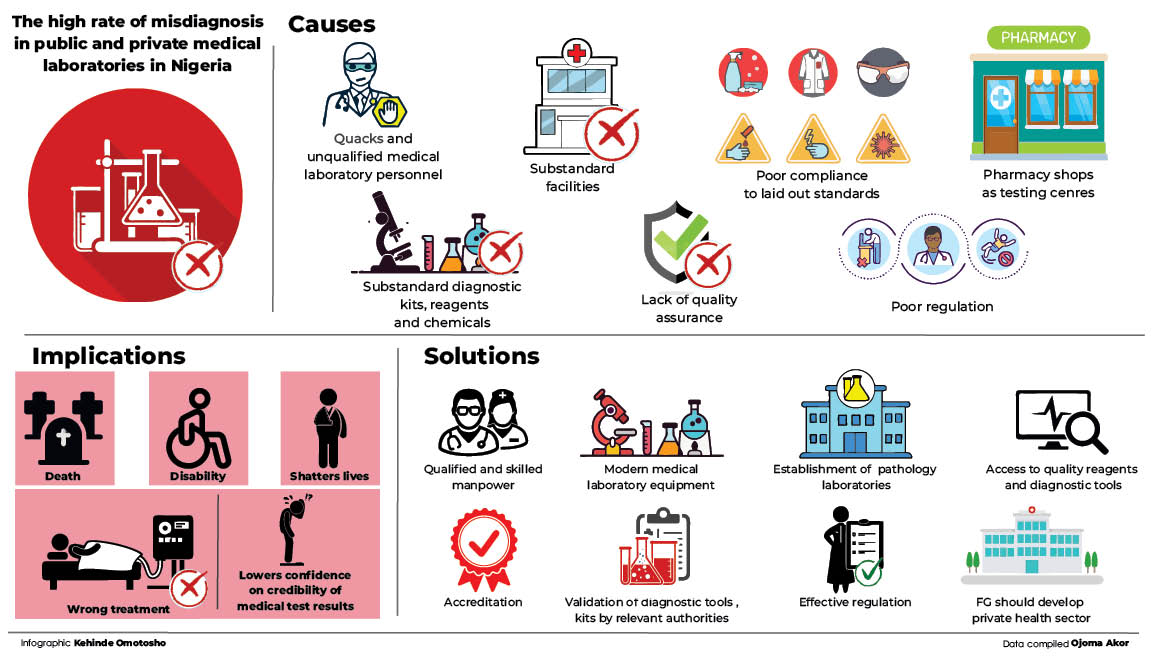
There are growing concerns over conflicting medical test results from private and public medical laboratories in the country.
Findings reveal that this has left in its wake, deaths and negative implications on the treatment and management of patients, as well as their general wellbeing.
- Suspended AGF compromised TSA, IPPIS, GIFMIS to ‘steal’ N109bn – EFCC
- THE BEARING: “How A Heartbreak Almost Ruined My Life”
Dr Ifeanyi Casmir, a medical laboratory scientist, said Nigeria was bedeviled with misdiagnosis and missed diagnosis.
Misdiagnosis is when a diagnosis has been made but is incorrect, while missed diagnosis is a situation where no diagnosis is made at all but the patient is ailing, Dr Casmir explained.
He said, “For example, if you have acute abdomen and they tell you there is nothing wrong with you, it is missed diagnosis. And if you are told you have pelvic inflammatory disease, then it is misdiagnosis, or wrong diagnosis if eventually what you actually have is ovarian cyst or cancer of the ovary.”
Casmir, who is also the immediate past publicity secretary of the Association of Medical Laboratory Scientists of Nigeria (AMLSN), said the cardinal determinants of medical results validity were precision, accuracy and reproducibility of the result.
“If you go to a medical lab to do lipid profile and go to another place, for example, in the United Kingdom and repeat the same test on the same person at the same time, and probably on the same sample and get the same value, that simply means the test is reproduceable,” he added.
For the purpose of this report, Daily Trust Saturday, with the assistance of some health experts, sent the same sample to different medical laboratories for malaria test, and different results were received the same day, with some having variations in the number of parasite count. Malaria is endemic in Nigeria.
Joseph Salifu David, a medical laboratory scientist, said the rate at which medical laboratories in Nigeria either misdiagnose, under-diagnose or over-diagnose malaria parasites (MP) was alarming.
He said lack of quality assurance accounted for different malaria results from different laboratories.
“The results are released with reckless abandon, with outrageous parasite count of two plus (++) and above.
“Malaria parasite test results are hardly reproducible in Nigeria. It is debasing that if you visit three laboratories for malaria parasite tests you will get three contradictory results.
“This lowers the confidence of clients on the credibility of the procedures employed on the tests, as much as it puts question marks on the proficiency of lab professionals,” David, who is also the immediate past chairman of the Federal Capital Territory (FCT) branch of the AMLSN said.

Misdiagnosis has dire consequences on patients’ care and management – NMA
The president of the Nigerian Medical Association (NMA), Dr Uche Ojinmah, said that in over 50 per cent of cases a doctor could make a diagnosis clinically by examining and talking with the person, among others.
He, however, said there were occasions where diagnosis would be dependent on a medical investigation result.
He said that in this case, the implication of misdiagnosis and missed diagnosis would be dire because “once the diagnosis is wrong, the treatment will be wrong automatically if you rely on it. For example, if someone has ring worms and you make a diagnosis of leprosy, you are bound to give treatment for leprosy not ring worm, and the ring worm will continue to fester.”
He said studies had shown that a lot of times, a case of missed diagnosis may take the patient up to two years to come back to the proper diagnosis.
Dr Ojinmah said missing a diagnosis could actually be a death sentence for someone, so it is vital to get it right.
He also said, “Some people have suffered immensely because they were given the wrong genotype results, leading to marriage of AS partners (without knowing they are AS) and ending up giving birth to children with sickle cell anemia.
“So some people have had that misfortune. They went to the lab and were told they were AA and they got married, only to find out later that the results were wrong.”
Experiences of some Nigerians
Titi Oladele needed a domestic help and decided to do pregnancy, HIV and hepatitis tests on the 19-year-old woman brought to her before employing her.
She took her to two different private medical laboratory facilities in Abuja for the test the following day.
She received negative results for all the three tests from the first laboratory while the medical result from the second lab showed positive results for pregnancy, hepatitis B and negative for HIV.
Oladele was confused on which of the tests to work with, especially as the would-be domestic servant wept profusely that she was not pregnant.
She recalled that when they got to the first laboratory, the person who did the test was also performing the role of a receptionist.
“When we asked of the medical laboratory scientist she told us he went out, but that she was also trained and could do the tests. She kept us waiting for so long for the result, and at the end, handed us an all negative result.” Oladele narrated.
The next day, Oladele took the young woman to another private laboratory to repeat the tests. This time, the result came out positive for pregnancy and negative for hepatitis B and HIV.
“I was confused on which medical result to rely on amongst the three but decided to tilt towards the last one. Since I didn’t want a pregnant house help, I decided to buy pregnancy test trips from a pharmacy on our way home and asked her to do it twice, and they both recorded positive results.
“I told her that I would not be able to employ her as she might not be able to handle the rigours that come with the job in her condition. It was then that she broke down and confessed that she actually knew she was pregnant.
“If I had relied only on the result from the first lab for the pregnancy and hepatitis B test, I would have been misled. The contradictory tests could also put me and my children at risk, especially as it showed negative for hepatitis B,” she added.
Chigozie, 37, decided to do some pre-marital medical tests with his fiancée at the medical laboratory of a public hospital in Abuja.
The medical results showed he tested positive for hepatitis B but negative for HIV, and all other tests he did.
He said, “I was devastated because I learnt that hepatitis B had no cure. I also feared losing my fiancée. In fact, it was one of the most traumatic times of my life because many people, including family members, advised my fiancée to call off the relationship so that she would not get infected. At that time, the knowledge about the condition and medicines to manage it were not available as it is now.
“While my relationship was shaky, I saw a doctor with the report and he prescribed drugs for me, which I started taking. We then postponed our wedding by a year. “
He said that after some time, the doctor asked him to do another test, and it came out negative. He repeated it twice outside the facility and it was negative.
“The summary is that I never had hepatitis B in the first place. So my doctor asked me to discontinue treatment.
“Before the discovery of the misdiagnosis, my fiancée and I went through a lot. I became depressed, coupled with the medicines I was taking, as well as the embarrassment of explaining to family and friends, the reasons for the postponement of the wedding. Though we are married now, it is not an experience I can forget in a hurry,” he added.
Mairo recalls that when she went for a scan during her pregnancy last year, a private facility told her she was carrying a boy, however when her doctor asked her to do a scan in the hospital where she was doing antenatal, she was told she was carrying a girl, after each scan. But she delivered a boy at the end of the pregnancy.
“I don’t know if it is the machine or the woman who did the scans was not qualified. I already had three girls then and was wishing for a boy, so the result made me anxious,” she said.
A woman who wants to be identified only as Mrs Haruna, said her late husband was diagnosed of ulcer in a public hospital. He was receiving treatment for over a year before a second opinion revealed that he had been suffering from colon cancer. He died shortly after that experience.
Reasons for conflicting results
Dr Casmir, the medical laboratory scientist, said the major reasons Nigeria is recording high cases of conflicting medical test results across public and private labs was because medical laboratory testing had become an all-comers affair, as well as poor monitoring compliance to laid out standards.
He said government and private facilities would employ people who had no business in the medical laboratory as a result of poor regulation, corruption and nepotism.
“So, when you have the wrong personnel providing medical testing, you get wrong results.
“You will be shocked that no teaching hospital or federal medical centre in Nigeria has International Certification (ISO) ISO 15189 accreditation for the laboratories they operate,” he said.

He lamented that pharmacy shops were also contributing to the menace as most of them in the country were providing testing.
“Pharmacies are not places for medical laboratory testing. So, if you go to a pharmacy to do test, you have patronised a quack. So, infiltration of quacks into testing in Nigeria is one of the reasons we have the predominance and endemicity of wrong and misleading test results,” he said.
He said another reason for misdiagnosis and missed diagnosis was because Nigeria had become the leading dumping ground across the globe for substandard rapid test and diagnostic kits, reagents and chemicals.
He said this is as a result of poor regulation and non-validation, adding that before test kits are deployed, the global standard practice is to be subjected to very serious scrutiny following international and local regulatory standards.
Dr Casmir said this accounted for the practice of many diagnosis ending as ‘typhoid and malaria’ results from these facilities. According to him, no hepatitis test kit has been validated in the country till date.
He said the federal government provided a regulatory frame work and gave the Medical Laboratory Science Council of Nigeria (MLSCN) the sole responsibility of approving and validating and registering diagnostic kits, reagents, chemicals for clinical laboratory diagnosis, testing of human beings, but many of these are being done in the country without recourse to the Council.
He said that in 2020, the MLSCN attempted to validate some of the Radio Diagnostic Test kits for COVID-19 but only two organisations passed the validation, while the rest failed. However, he added that these unvalidated test kits had been fully deployed and in use in the country.
MLSCN seals substandard labs
Some months ago, the MLSCN sealed 10 medical laboratories in the Federal Capital Territory (FCT) for unethical practices and non-compliance to operational standards during a three-day inspection exercise.
The deputy director, Practitioners’ Regulation And Discipline of the council, Ini Edeh, said, “While it is commendable to note that some medical laboratories in the FCT are operating in line with the regulations and were scored above average, the MLSCN inspection noted that many others were still operating below the minimum standard required to guarantee quality medical laboratory results.
“Furthermore, we also noted the use of unqualified medical laboratory personnel to generate laboratory test results by some facilities, while others operate under unacceptable facilities that compromise quality, as well as staff and patients’ safety.”
She said some of the qualified medical laboratory scientists and medical laboratory technicians did not have current practising licences and work permits respectively. Therefore, the MLSCN cannot guarantee the accuracy of the test results they generate.
She added that over 50 per cent of the inspected medical laboratories in the FCT did not participate in any External Quality Assurance (EQA) scheme.
“This also casts shadows on the quality of test results they produce,” she said.
Way out
To address the problem, the president of the Nigerian Medical Association (NMA), Dr Uche Ojinmah, said Nigeria needed to tilt more towards pathology laboratories than mushroom medical laboratory science laboratories that are not properly regulated or equipped.
He said, “We call on those who want to open medical laboratories to collaborate; one-man laboratory is not good because you don’t know who is doing the quality control.”
He also said medical doctors who are experts on laboratory investigations and interpretations were called pathologists, adding that they should be encouraged to go into private joint practice.
“Where you have a chemical pathologist, microbiologist and a haematologist, they can collaborate so that the haematologist would be in charge of blood tests and diseases, the chemical pathologist may be in charge of urine test and HIV screening etc, and the microbiologist looks for infectious diseases in the system.
“If we can have combined pathology laboratories, properly registered with ISO certification and the Nigerian Standard Organisation certification, it will be good.
“Synlab is the only pathology laboratory we have, and it is doing very well. The results you get from there because it has a standardised certificate can be used outside this country. So we look forward to having more,” he said,
He said that in the medical laboratory section, the scientist does bench work in the test process and also does routine investigation if in a teaching hospital, while the interpretation of the results and matching it to patients care is the business of a pathologist .

He, however, said that in the private sector, the pathologist could do a lab test and also read the result.
He said that is why pathologists should go into private practice so that they could employ the medical laboratory scientist to work on the bench while they would have the time to read the results.
The NMA president also called on the government to make funds available for the development of the private health sector as done in other countries, such as India.
Dr Casmir, the medical laboratory expert, called on the MLSCN to sanitise the practice, adding that the Pharmacist Council of Nigeria (PCN) should also sanitise the practice of pharmacy shops that metamorphosed into medical labs.
“They are endangering communities where they practise, not only those who go to them for test but also those who live around there,” he added.
Joseph Salifu David, the immediate past chairman of the Abuja branch of the AMLSN, said the mainstay of an efficient, effective and accurate diagnosis of malaria revolved around putting in place, a quality assurance programme.
He said medical laboratory scientists should adhere to standards and procedures in diagnosis in order to ensure quality results and public confidence.
“Although there may be several analytical methods, if all labs carry out their tests under the established controlled ambiance, observe the same principle and maintain the standard condition for each test, they will all produce the same result for the same client,” he said.
The registrar of the MLSCN, Sir Tosan Erhabor, said medical laboratory facilities needed to key into the global programme of accreditation to upscale their services and ensure accurate and reliable test results.
He said that in world over, health laboratory systems were increasingly embracing accreditation because it is a hallmark of quality in medical laboratories and other systems.
He said, “The time has come for every medical laboratory in the country to begin to benchmark international best practices through accreditation. Such has been instrumental to the accurate and reliable medical laboratory diagnosis we seek abroad; and if it is good for the citizens of other nations, it should be good for our citizens too. Currently, in some countries, no medical laboratory facility is allowed to operate without being accredited.”
He said the MLSCN was committed to supporting medical laboratories in the country willing to key into the process of accreditation, noting that that patients expect and deserve accurate and reliable medical laboratory results.
He said the council was also working towards a policy of mandatory accreditation for medical laboratories, especially for federal teaching hospitals and federal medical centres.
He said that with accreditation, the MLSCN as a national regulator could vouch for the quality of services at accredited facilities.
This report was supported by Daily Trust Foundation, with funding from the MacArthur Foundation.
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
