You could get really sick from COVID-19 while someone else doesn’t. Some people don’t even show symptoms at all. Nobody knows why.
A new study shows there may be deviations in immunity and lapses that determine the difference: whether a case of COVID-19 is severe or mild.
COVID 19: Katsina records 24 deaths, discharges 705
Low Covid-19 fatality rate, a big hope for India
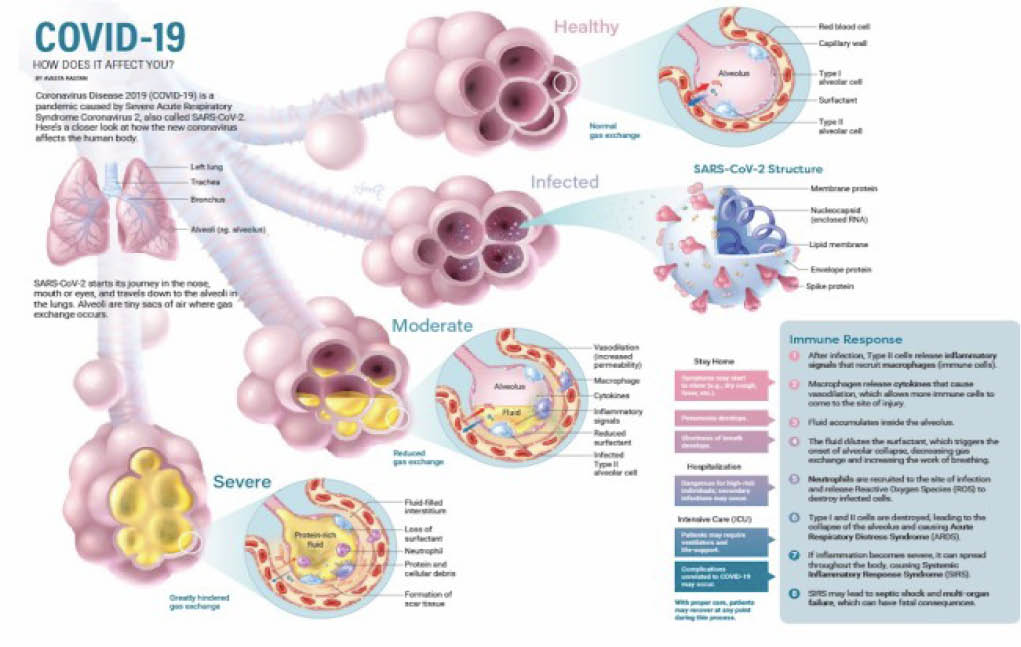
The innate immune system we have is ancient. But how it responds to SARS-CoV-2, the virus that causes coronavirus disease, matters.
The innate immune system is found in all creatures. It is your body’s defence mechanism—an army of soldiers ever ready to go into battle to protect your body.
It rapidly senses viruses and other pathogens. As soon as it does, it launches an immediate attack on them. This attack is indiscriminate at first. But then it mobilises more precisely targeted attack using cells you might consider as “sharpshooters”. Except these sharpshooters are slow to get moving. They actually belong to a different branch of the body’s pathogen-defence forces called the adaptive immune system.
“These findings reveal how the immune system goes awry during coronavirus infections, leading to severe disease, and point to potential therapeutic targets,” said Bali Pulendran, PhD, professor of pathology and of microbiology and immunology and the senior author of the study.
The study was done by investigators at the Stanford University of Medicine and other institutions and its findings published in the journal Science.
Lead authorship is shared by Stanford postdoctoral scholars Prabhu Arnunachalam, PhD, and Florian Wimmers, PhD; and Chris Ka Pun Mok, PhD, and Mahen Perera, PhD, both assistant professors of public health laboratory sciences at the University of Hong Kong.
Three molecular suspects
The researchers analysed the immune response in 76 people with COVID-19 and in 69 healthy people.
They found enhanced levels of molecules that promote inflammation in the blood of severely ill Covid-19 patients.
Three of the molecules they identified have been shown to be associated with lung inflammation in other diseases but had not been shown previously in COVID-19 infections.
“These three molecules and their receptors could represent attractive therapeutic targets in combating Covid-19,” said Pulendran, who is the Violetta L. Horton Professor. His lab is now testing the therapeutic potential of blocking these molecules in animal models of COVID-19.
Bacterial debris and immune paralysis
The scientists also found elevated levels of bacterial debris, such as bacterial DNA and cell-wall materials, in the blood of those COVID-19 patients with severe cases.
The more debris, the sicker the patient — and the more pro-inflammatory substances circulating in his or her blood.
The findings suggest that in cases of severe COVID-19, bacterial products ordinarily present only in places such as the gut, lungs and throat may make their way into the bloodstream, kick-starting enhanced inflammation that is conveyed to all points via the circulatory system.
But the study also revealed that key cells of the innate immune system in the blood of Covid-19 patients became increasingly paralyzed as the disease got worse.
Instead of being aroused by the presence of viruses or bacteria, these normally vigilant cells remained functionally sluggish.
If high blood levels of inflammation-promoting molecules set Covid-19 patients apart from those with milder cases, but blood cells are not producing these molecules, where do they come from?
Pulendran believes they originate in tissues somewhere in the body — most likely patients’ lungs, the site of infection.
“One of the great mysteries of COVID-19 infections has been that some people develop severe disease, while others seem to recover quickly,” Pulendran said. “Now we have some insights into why that happens.”
Pulendran is a member of Stanford Bio-X and a faculty fellow of Stanford ChEM-H.
Courtesy: Science
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


