Cervical cancer is the second most common cancer affecting women and girls in Nigeria. Despite the fact that Human Papilloma Virus (HPV) vaccine can prevent the disease, access to vaccination is very poor in the country, Daily Trust Saturday reports.
Halima Abubakar, 65, sold her house to meet up with treatment costs following her cervical cancer diagnosis last year. Before then, for almost four years she had been spending money from one health facility to the other with the diagnosis of ‘infection’.
She was finally diagnosed of cervical cancer after a pap smear test, CT scan and others at the Aminu Kano Teaching Hospital (AKTH) Kano in August last year.
She was thereafter referred to the National Hospital Abuja for chemotherapy (treatment that uses drugs to kill cancer cells) and radiotherapy (a cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumours).
FG appoints 11 CMDs for health institutions
Flooding: FG to release ecological funds to Ondo, others
Cervical cancer, also called cancer of the cervix, is a type of cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the womb, and it also connects the womb to the birth canal.
Abubakar said the pain of the disease, and burden of paying out of pocket for treatment is really taking a toll on her.
“Some relatives, friends and my children have supported me but the cost of treatment is far beyond what we can afford. The treatment is expensive, and I am not working; only doing some little businesses in the house,” she said.
She was asked to do another treatment called brachytherapy (a type of treatment that places radioactive materials inside the patient to kill cancer cells) over two months ago but has not been able to do so due to lack of money.
Eunice Ogochukwu, 42, went for a fibroid surgery in April last year but didn’t get better after a month. Rather, she felt more ill and received diagnoses of ulcer, fever, malaria when she visited the hospital.
In the following weeks, she told a doctor in one of the private hospitals she visited that she had noticed a growth on her thigh.
The doctor went on to examine her, carried out a biopsy (an examination of tissue removed from the body to check presence, or extent of a disease), and also asked her to do some tests.
“That was how I was diagnosed of cervical cancer, and referred to American Cancer Hospital, a private cancer treatment centre in Owerri, Imo State. The treatments have been very expensive. I have spent over N6 million,” she narrated.
She explained that the doctor wanted to refer her to a tertiary public health facility nearby but could not do so because the radiotherapy machine there was always breaking down, and not working for months on end, causing interruption and time waste in accessing treatment.
She has so far received four cycles of chemotherapy, five weeks of radiotherapy, and also did brachytherapy at the University of Nigeria Teaching Hospital (UNTH) Enugu.
Ogochukwu added that she was lucky to be alive because at some point, she almost died amidst the endless treatments.
However, she has lately been diagnosed of a swollen right kidney, (which she suspects to be side effects of the cancer drugs she was taking) and, degenerative changes in the spine following persistent complaints of severe waist pain.
She said she was in dire need of financial support for her treatments, and lamented that she had applied for a supposed government fund for cancer at the facility she was receiving treatment but that months after, nothing has come out of it.

Juliana Ige‘s mother died three years ago after a five-year battle with cervical cancer. The twenty-five-year-old lady read about HPV vaccine and regular pap smear screening on the internet.
She decided to get her little sister and cousins vaccinated but was surprised at the unavailability of the vaccine in the public and private hospitals she visited, as well as the high cost for a single dose in the facilities where they were available. It took her one more year to get only her sister vaccinated.
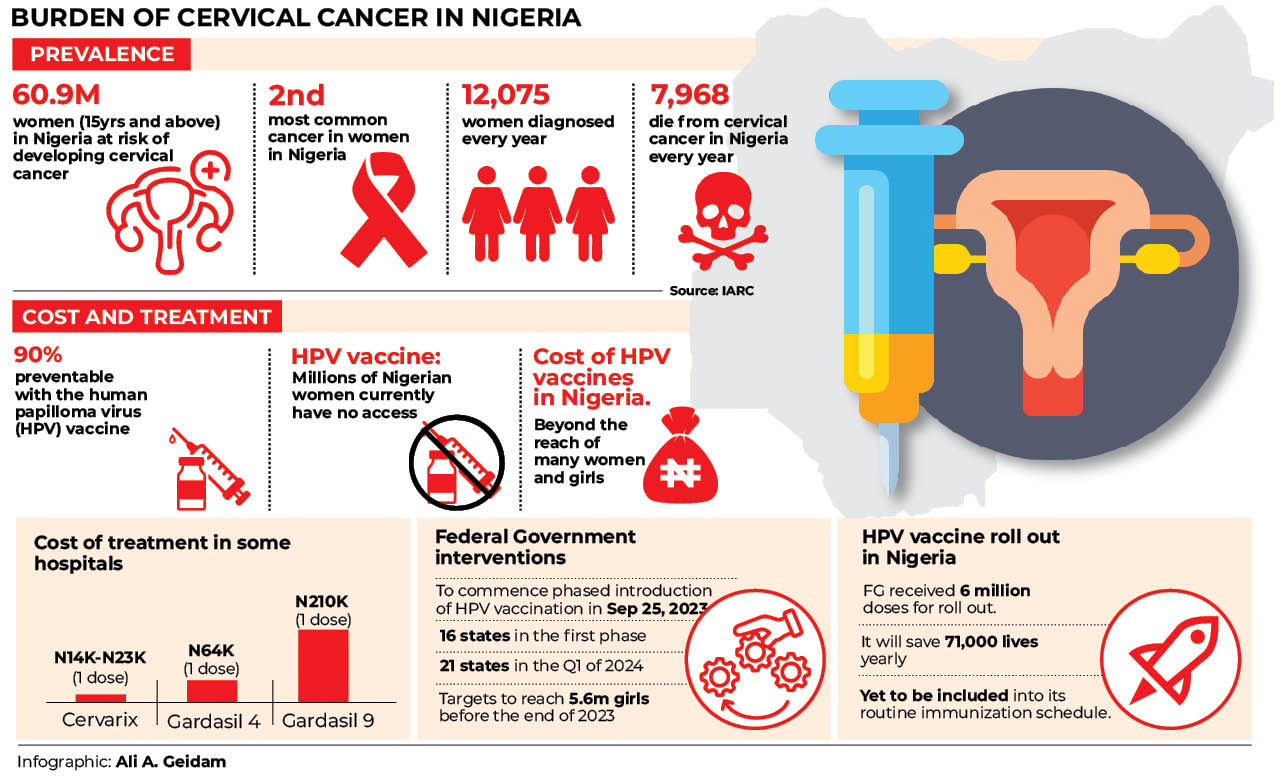
Nigeria has a population of 60.9 million women, ages 15 years and older, who are at risk of developing cervical cancer, according to the International Agency for Research on Cancer (IARC) 2023 factsheet.
The IARC data also reveal that 12,075 women are diagnosed of cervical cancer with 7,968 dying from the disease in Nigeria ever year.
The Human Papillomavirus (HPV) is a sexually transmitted Infection (STI) and has been implicated in over 90 percent of cases of cervical cancer.
Medical experts said persistent infection from HPV puts people at risk of cancers of the cervix, vulva, vagina, anus and throat in women, and cancers of the anus, mouth and penis in men.
HPV causes cervical cancer by infecting cells in the cervix, changing them and causing them to replicate and multiply in an uncontrolled manner.
Dr Ishak Lawal, a consultant Obstetrician and gynaecologist at the Federal Medical Centre Birnin-Kebbi, Kebbi State, said there is incontrovertible evidence that HPV infection is a trigger factor for cervical cancer, adding that this means that in 90 percent of cases of cervical cancer, there is that presence of HPV virus infection.
Lawal, who is also the Executive Director, End Cervical Cancer Nigeria Initiative, and Co-Chair- Women in Politics Against Cancer (WOPAC), said a major concern about the Nigeria situation is the fact that unlike developed countries, cervical cancer is almost a death sentence in the country because of many factors, such as late presentation for care.
Current state of access for women and girls to HPV vaccination in Nigeria
Medical experts say vaccinating girls and boys with the HPV vaccine before they are sexually active is the most effective way of preventing cervical cancer.
The World Health Organization (WHO) recommends that the vaccine is given to girls between the age of nine and 14 before start of sexual activity, and exposure to HPV and other sexually transmitted diseases.
However, despite this, millions of women in Nigeria have no access to the HPV vaccine.
The cost of getting the vaccine is usually beyond the reach of many women and girls, leaving them vulnerable to one of the most preventable and treatable forms of cancer.
Findings from health facilities during this investigation revealed that HPV vaccines was not readily available to those that need them, and many women and girls interviewed said they have never heard about HPV vaccines nor that it offers protection against cervical cancer.
Runcie Chidebe, Executive Director, Project Pink Blue, a cancer advocacy organization, said the fact that Nigeria does not have a HPV vaccination programme limited availability and access to it for women and girls.
He said it was only available to those who could afford to pay for it out of pocket. According to him, in 2021, Nigeria had a huge shortage of the HPV vaccine.
He said, “Nigeria is a poor country, so, with people struggling to eat, live or transport, it wouldn’t be easy telling them to buy a vaccine that costs a minimum of N15,000.”
He said in a global report released in March this year, Nigeria has blank spaces for men and women on the dashboard on HPV vaccine availability.
He said he believes strongly that the federal government’s announcement to introduce HPV vaccination this year will finally happen.
He said the roll out is important with the backdrop of over 25 per cent of the country’s population at risk of developing human papilloma virus, and with over 55 per cent of those with HPV that led to cervical cancer dying.
He said there are different types of HPV vaccines, adding that Cervarix costs N14, 000 for one dose, Gardasil 4 costs N64, 000 for one dose while Gardasil 9 cost N210, 000.
“You may require two or three doses depending on the advice of the doctor. How many Nigerians can afford this in a country where minimum wage or income is less than N30,000?” Chidebe added.
Dr Ishak Lawal, the consultant Obstetrician and gynaecologist, said COVID-19 caused disruptions in HPV vaccine availability and also delayed the roll out of HPV vaccination in Nigeria.
He said Cervarix, Gardasil 9 and Gardasil 4 types of HPV vaccines are available in the country now but mostly in private health facilities.
“The cheapest which is Cervarix, usually hovers around N15,000 to N30,000,” he said.
Asked the reasons for price difference in the HPV vaccines, he said Gardasil protects against four HPV viruses—that is HPV 16 and 18, which are the cancer-causing HPVs, as well the non-cancer-causing HPV 6 and 11.
He also said Cervarix protects against HPV 16 and 18.
He added that the National Primary Health Care Development Agency (NPHCDA) is planning to roll out Gardasil,
which is quadrivalent (protects against 4 HPV viruses).
Asked if women and girls older than 14 can take the HPV vaccine, he said “It is best given before puberty. However, using it after 14 years, is not harmful. The only thing is that the government cannot possibly provide HPV vaccine for everyone for free. The recommendation by WHO means every government must invest in providing this vaccine free for children between nine and 14.”
He said the vaccine can be given to male and female between nine and 14, adding that most developed countries are giving it to boys and girls.
He explained that males do not have cervical cancer—the most common complication of HPV infection so the best buy in for low-income countries like Nigeria is to give it to girls between nine and 14.
He said HPV vaccine also protects against other complications of HPV infection such as genital warts, laryngeal papilloma, laryngeal cancer and oropharyngeal cancer.
How HPV vaccination will save lives of women and girls in Nigeria
UNICEF Nigeria Chief of Health, Dr Eduardo Celades, says increasing access through introduction of HPV vaccination in Nigeria will help avert 71,000 deaths.
He said HPV vaccine protects in two ways, “protects you directly against the human papilloma virus (HPV) type 16 and 18, and as well as cross protection against other types.
“So, it is not only targeting these types that are very much prevalent in Nigeria, but also gives some sort of cross protection against all types, so it gives quite a lot of protection.”
He said, “We expect at the end of the vaccination 83 percent reduction of the probability of getting a cancer due to HPV.
“So, when we put that in the Nigerian context, it means that 71,000 deaths are going to be averted.”
Dr Ishak Lawal of the End Cervical Cancer Nigeria Initiative, said “all science has pointed to the fact that if we are able to vaccinate girls with HPV vaccine, it will significantly reduce their chances of having cervical cancer in the future.”
He said this means that the country will be saving the lives of those 7,000 women and girls that die from cervical cancer annually.
WHO Nigeria Country Representative, Dr Walter Kazadi Mulombo, said introducing HPV vaccination will save a lot of lives, and millions of lives in the future.
He said the vaccine is very effective and if introduced and implemented correctly, will help make the huge burden of cervical cancer disappear over time.
Founder of Medicaid Cancer Foundation, and immediate past First Lady of Kebbi State, Dr Zainab Shinkafi Bagudu, is one of the major persons that has been calling on the federal government to include HPV vaccines in the country’s routine immunization schedule over the years.
Bagudu, who is also member of the Union for International Cancer Control (UICC) Board of Directors, said “One of the ways of reducing the incidence of cancer in Nigeria is to make available free cervical cancer vaccines for young girls and boys before they become sexually active. The models used for polio vaccination can be easily adapted,” she advised.
Also, First Ladies Against Cancer (FLAC), a coalition of the spouses of current and former state governors working against cancer, has persistently expressed concern over the unavailability of HPV vaccines for millions of Nigerian girls through primary healthcare facilities in the country.
The cancer survivors Eunice Ogochukwu, and Halima Abubakar said cervical cancer is a disease that has gone ‘viral’ based on the number of people affected that they see in hospitals or around them.
They advised that the vaccine should be made readily available, and that parents should get their children vaccinated against the disease.
They also called on government to support the treatment of those who already have the disease.
Runcie Chidebe, the cancer advocate and executive director of Project Pink, says treating cervical cancer patients brings a lot of economic burden on the country.
He said government should invest in prevention because it is cheaper than treatment.
“It costs almost N3m to N7m to treat one cervical patient, and this amount is spent by both the individual and the government because the government has to provide the hospital support, and treatment machine, among others.”
He said this is in addition to the fact that the children of most women with cervical cancer have to abandon their work to take care of them.
“These are young people that should be contributing to the economy, but have become care givers. I have a friend whose mother had cervical cancer. The business the young man was doing collapsed because he had to be going to the hospital frequently,” he added.
Gloria Orji, a cancer survivor and President, Network of People Impacted by Cancer in Nigeria (NEPICIN), said “It is by introducing HPV vaccination that more girls will have improved access to the vaccine. With the poverty level in the country, if that is not done, more women and girls will continue to die from the disease.
“If the HPV vaccine is rolled out, and we are able to vaccinate our girls of the stipulated age, they will be sure of a cervical cancer free future where they wouldn’t experience the sufferings that come with the disease.”
Introduction of HPV vaccine in Nigeria’s routine immunisation
The government of Nigeria has been unable to include HPV vaccine in the routine immunization schedule after many promises over the years.
However, it announced early this year that it will commence a phased introduction of the vaccine in the country’s routine immunisation schedule this year, with the support of Gavi, UNICEF, World Health Organisation (WHO) and other partners.
There are strong indications that it would commence the roll out of HPV vaccine this time around.
Experts have welcomed the development and also advised on measures that need to be put in place to ensure access to the vaccine for all those that should receive it, as well as sustain the roll out.
The National Primary Health Care Development Agency (NPHCDA) said the first phase of HPV vaccine introduction in the country will commence with 16 states on 25th September.
The states are Abia, Adamawa, Lagos, Akwa Ibom, Bayelsa, Nasarawa, Jigawa, Ogun, Taraba, Kano, Benue, Osun, Federal Capital Territory (FCT), Kebbi, Bauchi and Enugu.
The other 21 states are expected to commence in the first quarter of 2024.
The Executive Director of the National Primary Health Care Development Agency (NPHCDA), Dr Faisal Shuaib, said “the introduction of HPV vaccines signifies our commitment to promoting preventive healthcare and empowering our population, especially our young generation, to live healthier lives. We recognize the immense value of prevention in reducing the burden on our healthcare system, sparing individuals from unnecessary suffering and ultimately saving lives.”
How UNICEF is supporting HPV vaccination roll out in Nigeria
UNICEF Nigeria Chief of Health, Dr Eduardo Celades, said Nigeria has already received 6.04 million doses of Gardasil HPV vaccine with the financing support of Gavi while UNICEF handled the process of procurement and shipment to Nigeria.
“The target is to reach 12.3 million girls with HPV vaccination,” Celades said, adding “Our target is to reach 5.6 million girls before the end of the year.”
“After doing a massive campaign to reach these girls from nine to 14 years old, then HPV vaccine from 2024 onwards will be routinised,” he added.
While saying routinising HPV vaccination in the country is going to be a game changer, he said UNICEF is working very closely with the NPHCDA and the Federal Ministry of Health and partners like GAVI to make it happen.
He said UNICEF was supporting the 16 states rolling out this year with micro planning, as each state needs to plan how it is going to reach the girls.
He said UNICEF was also supporting with the community engagement of girls, adding that there was a dual strategy one targeting girls in schools, and the other girls out of school.
“And to do that, we are also working with traditional leaders, parents, teachers, communities and even hope to engage celebrities, influencers and people respected in the communities.”
He said they are working very closely with the communities involved in other to reach girls that are in difficult to reach areas.
How to ensure effective roll out and access to HPV vaccines in Nigeria
Runcie Chidebe said the government and NPHCDA needs to be innovative in terms of resource mobilization, and shouldn’t continue the old way of just getting vaccines from donors and giving to people.
“We need to be innovative on where we can get money from even Nigerians. We did it during COVID-19 where billions of dollars were raised.”
He said another one is research and evidence generation, adding that lack of data is still a big problem in the country.
He said there is need for accountability in the HPV vaccine roll out. “We should build strong accountability in a way corruption will not thrive with the HPV vaccine roll out,” he advised.
Chidebe said there is also need for Nigeria to commence local production of vaccines to ensure availability to those that need it.
Need to tackle mistrust, hesitancy against the vaccine
Dr Lawal, Executive Director, End Cervical Cancer Nigeria Initiative, said “There is a lot of mistrust in the system. So, if we are not able to get the people to be on our side to understand the value and importance of the HPV vaccine, then we might not be able to get it across to them.”
He said the fact that the HPV vaccine is given to adolescent girls could raise connotations on population control based on previous experiences with other interventions.
He said there is need to actively educate the people and maintain trust, and also put in place measures to reach girls in hard-to-reach areas where there is insecurity, flooding, inaccessible roads and out-of-school children.
While saying that HPV vaccination program requires collective action from everyone, he called for more robust stakeholder engagement including scaling up media and non-governmental agencies involvement.
Dr Lawal said, “For us, at the Nigerian Cancer Society (NCS), and the End Cervical Cancer Nigeria Initiative, our biggest worry is that we have waited far too long for this vaccine to come in. And it is going to be very disappointing for us if the vaccines now comes into the country and for one reason or the other, we are not able to give it to the right people.
“We expect some vaccine hesitancy. We know there is going to be some pushback. And if we allow that pushback to now prevent us from getting the benefit of this vaccine to the people, it is going to be really sad considering how long we have waited for the vaccine.”
He advised parents to protect the future of their girls, and the girls themselves should also protect themselves by ensuring they make themselves available for HPV vaccination.
This report was supported by the International Women’s Media Foundation’s Global Health Reporting Initiative: Vaccines and Immunization in Africa, in partnership with Sabin Vaccine Institute.”
This report was supported by the International Women’s Media Foundation’s Global Health Reporting Initiative: Vaccines and Immunization in Africa, in partnership with Sabin Vaccine Institute.
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


