The significantly more transmissible Delta variant means even higher numbers will have to be fully vaccinated to achieve any sort of herd immunity.
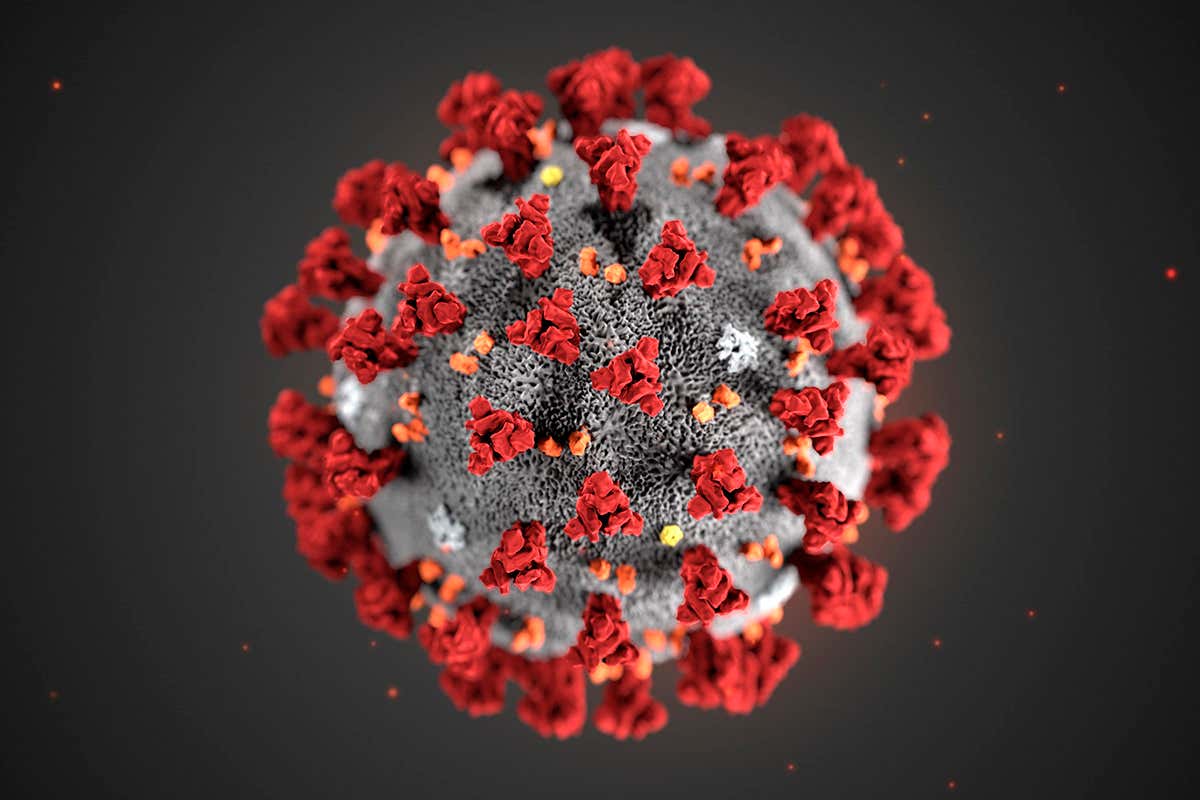
Herd immunity is a term that has been bandied around since the beginning of the coronavirus pandemic. It occurs when a large proportion of a population becomes protected against or immune to infection, significantly reducing the spread of that infection even in the unprotected group.
- We can win Champions League at PSG – Messi
- Yahaya Bello appoints Runsewe head Advisory Committee on Culture and Tourism
It can be achieved through the following:
Natural infection: when enough of a population has caught the infection and built up naturally acquired antibodies to the disease that protect against infection in the future
Vaccines: when enough people in a population have been vaccinated against a disease, allowing them to build up protective antibodies, without the need for infection, that are effective in protecting against serious infection in the future
When it comes to COVID-19, we know that trying to aim for herd immunity through natural infection can have devastating consequences. We have seen how the virus can rip through countries, leading to more than 4.3 million deaths worldwide to date. Not only this, it can cause serious illness in the acute phase, and impact lives and livelihoods with the effects of long COVID. We also do not know how effective antibodies acquired through natural infection are, or how long they last, and there are many cases of people catching the coronavirus more than once.
Vaccines, on the other hand, have successfully controlled contagious diseases such as smallpox, polio, diphtheria, pertussis, rubella and many others without the need for people to get sick. Whereas it is not uncommon for those vaccinated against COVID to experience mild, short-term side effects after getting their shot, unvaccinated people are far more likely to develop severe illness if they catch the virus.
We know that vaccines offer better protection than natural infection, with antibodies lasting longer and being more effective against serious illness. The World Health Organization (WHO) supports achieving herd immunity through vaccination, not by allowing a disease to spread through any segment of the population, as this would result in unnecessary cases and deaths.
It is also worth noting that the route taken towards “herd immunity” through vaccination is important; it is vital that the most at-risk groups in a population are vaccinated first as these people stand to lose a lot should they get infected. In the case of COVID, this means vaccinating the elderly and those with underlying health conditions first – offering them a level of protection while herd immunity is being achieved.
Although it makes sense to try to achieve herd immunity through vaccination programmes, there are challenges. First, just like naturally acquired antibodies, we are unsure how long protection from vaccine-induced antibodies will last, and more research is needed to ascertain whether the vaccines help reduce transmission of the virus.
Then, there is the matter of vaccine hesitancy and the spread of misinformation, which is preventing large numbers of people from taking up the vaccine.
But, the biggest challenge is the uneven distribution of vaccines across the world. As the most affluent countries rolling out effective vaccination programmes for their own populations, this leaves many poorer nations without vaccines and open to huge waves of infections; perfect breeding grounds for new variants to arise that could be resistant to the effects of the original vaccines.
The very idea of ‘herd immunity’ itself is a false concept when it comes to COVID. We have seen how antibodies naturally acquired through infection do not make you ‘immune’ to the virus and many people have reported getting second infections … For COVID, protection rather than immunity is a more realistic concept.
The exact percentage of a population that needs to be vaccinated against COVID to achieve herd immunity is a point of scientific debate. Generally speaking, the more infectious an illness is, the higher the percentage that needs to be vaccinated in order to achieve herd immunity. For example, herd immunity against measles requires about 95 percent of a population to be vaccinated – this is because measles is a very infectious disease. The remaining 5 percent will be protected by the fact that measles will not spread among those who are vaccinated. For polio, the threshold is about 80 percent as it is less infectious.
The proportion of the population that must be vaccinated against COVID to begin inducing herd immunity is not known. This is an important area of research and will likely vary according to the community, the vaccine, the populations prioritised for vaccination, and other factors. But the coronavirus that causes COVID-19 is incredibly infectious, with the main route of spread being airborne particles that linger in the air for hours and can be breathed in.
Of course, the Delta variant being up to 60 percent more transmissible has altered the trajectory of the pandemic, meaning even higher numbers than originally thought will have to be fully vaccinated to achieve any sort of herd immunity. Some scientists put the percentage of people needing to be vaccinated against Delta at 88 percent or above to achieve herd immunity, something that may not be possible given the challenges outlined earlier and the fact that the vaccines are less effective against the Delta variant than they are against the original variant and the Alpha variant.
The very idea of “herd immunity” itself is a false concept when it comes to COVID. We have seen how antibodies naturally acquired through infection do not make you “immune” to the virus and many people have reported getting second infections. The same is true for the vaccines; their aim is not make those vaccinated “immune” to the virus but to protect them against becoming seriously ill should they contract the virus. This is different to previous vaccination programmes, such as for measles and smallpox, where vaccines did confer immunity to the disease.
For COVID, protection rather than immunity is a more realistic concept.
The key is to get as much of the global population vaccinated as quickly as possible, including younger age groups like 12- to 15-year-olds. It makes sense that those vaccinated will manage to fight off the virus, due to their vaccine-induced antibodies, before it has a chance to divide and multiply inside them to numbers that allow it to spread to others.
It may be that, like the flu virus, we do not aim for herd immunity but rather maximum population protection through vaccines. To be frank, protecting people from serious illness and preventing healthcare systems from being overwhelmed may have to be enough.
Progress Report: WHO calls for countries to delay COVID boosters
Countries such as the UK, Germany and Israel have made it clear that they intend to begin giving a third booster COVID shot to vulnerable groups to help bolster their protective antibodies. Israel has already begun its booster programme and the UK will do so in September ahead of the winter period. However, there is growing concern that these booster vaccines will come at the expense of poorer nations, who are struggling to get enough vaccines to be able to vaccinate significant numbers of their populations. Some parts of Africa, for example, have only managed to vaccinate 2 percent of their population.
The WHO has expressed concerns over booster shots, and released a statement asking richer countries to pause them until the end of September at the earliest, in order to enable at least 10 percent of the population of every country to be vaccinated. In its statement, it went on to say: “To make that happen, we need everyone’s cooperation, especially the handful of countries and companies that control the global supply of vaccines.”
It called on “everyone with influence – Olympic athletes, investors, business leaders, faith leaders, and every individual in their own family and community – to support our call for a moratorium on booster shots”.
This comes on the back of the US Centers for Disease Control (CDC) saying it does not feel fully vaccinated Americans need booster shots, though it will continue to examine the evidence around this as it emerges. Europe’s health regulation agency, the EMA, meanwhile, has said it is too early to know if booster shots are needed because there is not yet enough data from vaccination campaigns and ongoing studies to understand how long protection from the vaccines will last.
The pandemic and race to vaccinate have highlighted the huge health inequalities that already existed across the globe. But what those countries racing towards booster shots at the expense of poorer nations must not forget is that they may well be paving the way to further variants. As large swathes of the globe remain unvaccinated, it creates pools of people for the virus to infect. When the virus infects more people, it has more of an opportunity to divide and spread further. The more it divides and replicates, the more chance of a mutation occurring that makes it resistant to the immune response triggered by the current vaccines.
If that happens and this new mutated variant finds its way back to the richer countries, it will undo all their good vaccine work. This means a cycle of needing more boosters against emerging variants.
It does indeed make more sense to prioritise the unvaccinated, but for that we need wealthier governments to exercise compassion for those who live in other countries, something that has often proven difficult for those in power to do.
Dr Amir Khan Aljazeera features
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.


