By Ojoma Akor, Nigeria & Haitham Alqaoud, Yemen
Severe acute malnutrition has continued to ravage children in conflict settings, such as Borno State in North East, Nigeria, as well as Hajjah and Hodeida governorates in Yemen.
In some cases, children under five, who were treated and discharged from outpatient and inpatient outlets relapse and return for the same treatment.
Umar Modu, 3, was discharged as having been cured of severe acute malnutrition six months ago, but he relapsed and is back at the Shuwari Outpatient Therapeutic Programme (OTP) in Jere, Nigeria’s north-eastern state of Borno, where he was earlier treated.
The facility is run by the International Medical Corps (IMC), Nigeria, a United States Agency for International Development (USAID)-funded programme.
“He fully recovered and was discharged last year. After six months, he began to suffer from diarrhoea and other symptoms again. We went to the hospital and he was given some medications, but he didn’t get better. We returned to the Shuwari OTP centre and he was diagnosed with severe acute malnutrition. He is now undergoing treatment,” his mother, Falmata said in Shuwa Arab language.

She said there was no disease outbreak in her neighbourhood during the time her child relapsed, and he had so far not been diagnosed with any other disease aside severe acute malnutrition.
Falmata has been living at the Shuwari police station internally displaced persons (IDP) camp since insurgents attacked her community six years ago.
Both Falmata and her husband were smallholder farmers in Dala before they were uprooted from their home by the violence. They have not been earning income since then and depend on food occasionally distributed by Save the Children International.
But such a handout barely meets the nutritional upkeep of her family. “I just cook whatever food I get and everyone in the household eats,” Falmata said.
Her household’s diet remained the same, in addition to poor water and sanitation facilities in the camp. A few months after Umar’s treatment, he relapsed.
Relapse means to fall back into illness after a period of improvement or recovery. Someone is said to be experiencing severe acute malnutrition relapse if the disease returns or the person suffers an onset of symptoms again after improvement.

Many children who have been cured of severe acute malnutrition in Nigeria and Yemen have been in the cycle of returning to the same treatment all over again as the conditions that caused their illness never changed.
This predisposes the children to death. Those that survive face life-long disabilities as they may never realise their full potential.
The right thing to do is to never let the children be malnourished, according to early childhood development experts.
And if they are ever acutely malnourished, they should be treated and prevented from relapsing. But their conditions in north-eastern Nigeria and Yemen are dire due to protracted violence that has killed thousands of people and displaced millions of others.
In Nigeria’s North East, where Islamic militants have waged war against government forces since 2009, there is no comprehensive data on severe acute malnutrition relapse.

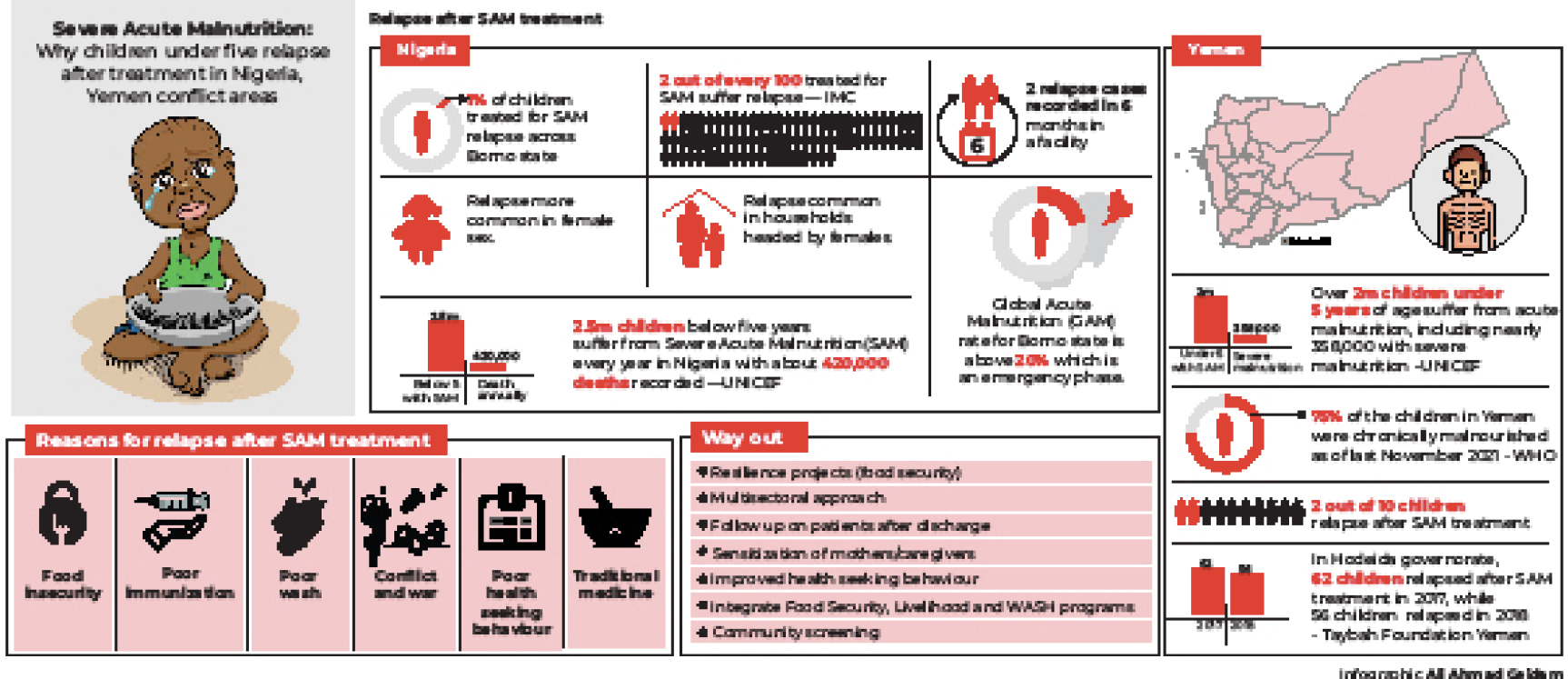
A 2020 study on incidence of severe acute malnutrition relapse in Nigeria’s north-western state of Sokoto shows that about 24 per cent of children cured of the disease in health facilities relapse within six months. The study was led by a team of researchers at Oxford Policy Management and Valid International, in collaboration with the United Nations Children’s Fund (UNICEF), Nigeria.
So far, no survey has been conducted on cases of severe acute malnutrition relapse in Borno State, the epicentre of insurgency, according to multiple health workers in the state who were interviewed.
“Out of 100 children cured of severe acute malnutrition, two suffer relapse,” said Dr Olusegun Ojetola, the nutrition programme coordinator, International Medical Corps who oversees the Shuwari and Jabbamari OTP centres and others in Borno.
He observed that most of the relapse cases occurred in female children and households headed by women.
“The mother does not have enough source of income to procure nutritious foods to prevent her child from returning to the facility malnourished,” he said.
In Yemen, data obtained from the Taybah Foundation for Development, which has been implementing its nutritional programmes under the UNICEF fund in the Hodeida Governorate, shows show that 62 children relapsed after severe acute malnutrition treatment in 2017, while 56 children relapsed in 2018.
Akram Alhalaly, who treats children with severe acute malnutrition in Abs Hospital in Hajjah Governorate, said two out of 10 children who had been treated for the disease returned to the hospital with the same condition after three to six months.
A debilitating disease of poverty, deprivation
In recent years, programmes have been put in place to treat severe acute malnutrition in Nigeria and Yemen. In Nigeria, for example, children with the condition are usually treated through an outpatient therapeutic programme of the Community‐based Management of Acute Malnutrition (CMAM). But some of the children who have been treated still face the risk of relapse.
A four-year-old Fatima Haroun was treated for severe acute malnutrition and discharged four months ago at the Jabbamari OTP camp in Borno’s capital, Maiduguri, run by the International Medical Corps. She suffered a relapse and is now on another treatment at the facility.
Her mother, Bintu Muhammad said Fatima had never been diagnosed with any co-morbidities or an underlying illness.
Muhammad said she was no longer working as a cleaner in a private school and her husband earned very little from his job as a labourer.
“Her condition refused to go because we are not getting enough food. We need financial support and capital to start a means of livelihood so that we can provide for her and treat her once and for all,” she said.

At the home of Hauwa Muhammad, a widowed mother of a 17-month-old Fatima Ali in the Ngomari area of Maiduguri, a case of severe acute malnutrition relapse has been daunting.
Hauwa said her daughter had faced a nine-month ordeal battling severe acute malnutrition and tuberculosis.
She said that Fatima was diagnosed with severe acute malnutrition at a hospital and subsequently referred to a therapeutic feeding stabilisation centre.
However, sometime after the child was discharged, she was diagnosed with tuberculosis at the Umaru Shehu Hospital in Maiduguri.
“She added weight and got better after the severe acute malnutrition treatment but relapsed after she developed tuberculosis, so we had to go back to the health centre for treatment a second time,” she said.
Fatima’s treatment involved ready-to-use therapeutic food (RUTF), a peanut-based paste in a plastic wrapper, which her mother used to feed her at home.
After the health workers confirmed Fatima’s cure, she was no longer qualified to get the RUTF. But without access to nutritious meals, she starved and relapsed.
“Since my husband died, we have been struggling to eat. Even when he was alive, we barely ate a day. So, his demise aggravated our plight. Sometimes we get something to feed on and sometimes we go to bed hungry,” Hauwa said.
Other areas across the state are also recording a high rate of severe acute malnutrition relapse.
“You will hardly go to any displaced persons camp like this without seeing cases of severe acute malnutrition relapse, particularly with the stoppage of food distribution by the government and non-governmental organisations,” Alhaji Musa Ajere, the chairman of Doro displaced persons camp in Maiduguri said.
In Yemen, an increasing number of children are also facing relapse. Waleed, whose parents did not want to be fully identified, had been suffering from fever, diarrhoea and anorexia when he was taken to the hospital.

In Abs Hospital in Hajjah Governorate, he was diagnosed of severe acute malnutrition. But two months after his successful treatment, he relapsed and returned to the hospital for another round of treatment.
“My son began to suffer from diarrhoea and became skinnier. His bones were too visible because he was vomiting many times. I borrowed money from my relatives to take him back to the hospital because I could not endure seeing him in so much pain,” Waleed’s mother said.
Apart from household food insecurity, their village, Beni Hassan in Hajjah Governorate lacks access to clean drinking water and sanitation.
“We don’t have any other source of water except the well. We used to receive chlorine tablets for water purification in the well, but now we no longer receive those tablets,” she said.
Salah, another child under five, has relapsed three times after treatment. He has been underweight since birth and was diagnosed with severe acute malnutrition at Althawarh Hospital in Hodeida Governorate, a nine-kilometer journey from their home.
His mother said that as a result of his condition, she planned to sell some of her home appliances to pay for his medical bills at the closest private hospital.
“My husband stopped receiving salaries for the past five years, leaving us with inadequate food daily,” she said.
Investigations revealed that millions of children in Nigeria and Yemen suffer from severe acute malnutrition.
According to the UNICEF, in Nigeria, about 2.5million children below five years suffer from such condition, with about 420,000 deaths recorded.
A December 2020 UNICEF report predicted a surge in such cases in North East, Nigeria and across Yemen. Also, last December, Doctors without Borders/Medecins Sans Frontieres (MSF) had treated exceptionally, a high number of children with severe acute malnutrition in Borno, more than the previous year.
Yemen has some of the highest malnutrition rates in the world.
The war in the country has left about 23.7million people in need of urgent humanitarian assistance, with more than 2 million children malnourished.
The UNICEF said that across Yemen, over 2 million children under five years of age suffered from acute malnutrition, including nearly 358,000 with severe acute malnutrition – a number that is expected to rise. Seventy-five per cent of the children in the country were chronically malnourished as at last November, according to the World Health Organisation (WHO).

In northeastern Nigeria, United Nations agencies estimated that about 3.2million children would face malnutrition this year.
In Borno alone, the acute malnutrition rate is above 20 per cent, and it is considered an emergency.
Dr Khawla Jabr, who treats severely malnourished children in Althwarah Hospital in Hodeida Governorate, said if the conflict in Yemen continued, a large number of children would be malnourished in many areas.
“The economic situation is bad and people cannot afford to get treated in private hospitals, therefore, Al-Thawrah Hospital is overcrowded with severely malnourished children,” Dr Jabr said.
She said malnutrition was complicated by the failure to receive basic vaccines in early childhood, adding that “malnourished children have weak immunity. So they are susceptible to many other diseases and infections.”
Yemen is also facing regular outbreaks of measles, diphtheria and other vaccine-preventable diseases. Immunisation coverage has stagnated at the national level, with 37 per cent of children under one year of age missing routine vaccinations, according to the UNICEF.
Reasons for relapse after treatment
Safiya Yunus, a nutrition officer at the Shuwari OTP site treating Umar Modu said about two relapse cases were recorded in six months in the facility.
She said children that relapsed so far did not have co-morbidities; that is the existence of more than one disease or condition in an individual at the same time.
Safiya said poverty and food insecurity had been the dominant factors in most of the cases they have seen.
“Insurgency is contributing to relapse because most of our beneficiaries are in displaced persons camps and have no source of livelihood.
“They depend on whatever food non-governmental organisations give them, and because they may be so many persons in their households, the quantity of food would not be enough for the family for a whole month. So, they have to manage within that month,” she said.
She said the facility also observed relapse in children from homes and areas with poor hygiene and in children with poor immunisation.
Ifeanyi Bartholomew Ojiaku, a nutrition assistant and team leader, Jabbamari OTP, where Fatima Haroun is being treated, said relapse in the facility was between two and three cases in six months.
He said children that had relapsed so far in the facility had no co-morbidities or underlying illnesses. However, he said poor personal hygiene and food insecurity contributed to cases they had seen.
He said they followed up on the children after discharge and had volunteers that do the bi-weekly follow-ups for beneficiaries that had already been discharged.
“We do one-on-one counselling at the time of discharge via the infant and young child section and give them advice on how to protect their children from relapse,” Ojiaku said.
Olive Muthamia, a humanitarian nutrition advisor at the Save the Children International, Maiduguri, said about one per cent of beneficiaries came back with relapses after severe acute malnutrition treatment in the organisation’s sites.
While pointing out that food insecurity is a contributory factor to the relapse cases, she said when the children were in the acute malnutrition treatment programme, they would have access to therapeutic foods, but when they are out of it, that source of food is no longer there.
She added that another contributory factor to relapse was caregivers taking their children to traditional medicine practitioners for treatment.
“There are some children that come back to our programmes after every two months. At that point, you have to refer them to the stabilisation centre for further investigation to establish if it is just food or there is another underlying medical condition making them relapse,” she said.
Muthamia said they had seen co-morbidities in some of the affected children, adding that sometimes during the rainy season, diarrhoea, malaria and pneumonia are the co-morbidities they witness.
During a recent visit to the Medecins Sans Frontieres (MSF)-Belgium therapeutic feeding centre for malnourished children in Maiduguri, Borno State, Nigeria, there was no relapsed child on treatment.
The 120-bed facility called Nilefa Keji (meaning health is wealth in Kanuri language) is the largest hospital and single provider of care for malnutrition in Borno State.
Musa Tanko, a data analyst/activity manager at the MSF said that in 2021, the facility recorded less than one per cent relapse rate in the inpatient therapeutic feeding centre, while 0.3 per cent of relapse rate was recorded in the ambulatory therapeutic feeding centre.
However, he said that in 2018, the facility had a higher relapse rate of more than one per cent, adding that most of the relapse cases in the facility had underlying illnesses such as tuberculosis and retroviral diseases.
Sangita Jacob Duggal, nutrition manager, UNICEF, Nigeria, Maiduguri field office, said the rate of relapse was small and below one per cent.
She said once the children were treated and cured, they would go into the next phase, which is moderate acute malnutrition before becoming finally cured.
She said it was a problem when the child was cured of severe acute malnutrition and discharged but did not get the basic minimum required care and the treatment protocol for home care.
Duggal explained that if the child doesn’t go through that process and has an episode of diarrhoea or any sickness, and the mother is not able to feed the child properly, “the child comes back to the severe acute malnutrition category, and that is where the challenge is.”
She said families had to understand that after discharge, the children would require support like more feeding, active care, including drinking water, hand-washing, among others.
Akram Alhalaly, the health worker at Abs Hospital in Hajjah Governorate in Yemen, which is supported by the MSF, said malnourished children are exposed to an unhealthy environment after they had been cured, which often resulted in relapse.
Dr Basma Al-Qadasi, a clinical nutrition and dietetics specialist in Alwaha Medical Center, said many children relapsed after treatment because they had many diseases like celiac, a defect in the intestines or frequent diarrhoea.
“Unfortunately, some nutritionists do not give full instructions to the mother about nutrition and do not practise optimal nutritional advice,” he said.
How to prevent relapse in children after treatment
Sangita Jacob Duggal of the UNICEF said one very important way was empowering families of children who are admitted to stabilisation centres.
“We are trying to introduce a mother corner or caregiver corner in the stabilisation centre, where we also give some kind of education or know-how skills on how to prepare energy-dense food items, using locally available food at home,” she said.
She said it was also important for health workers to keep track of discharged children so that they do not fall back into the acute malnutrition category again.
On the alleged diversion of the RUTF meant for the children, she said that across the world, wherever there is food insecurity, misuse and intra family distribution of the therapeutic food is rampant.
She said the UNICEF was trying its best to resolve it at the community level by training stabilisation facility workers and doctors to give some kind of guidance to the mothers who are staying there for 10 days or more to make use of all the products they get for the child alone.
She said UNICEF’s intervention when children under five relapse was to treat them again, adding that the target is to prevent any kind of malnutrition.
“If we have so many children suffering from severe acute malnutrition, it means we are failing in preventing malnutrition, and prevention is very much under the control of the family,” she said.
Ojiaku, the nutrition assistant and team leader, Jabbamari OTP, said sensitisation on personal hygiene and proper immunisation would help to prevent relapse after treatment.
“The issue of food insecurity should be reduced so that after discharge, the beneficiary can also have access to food in case it is not available in the house,” he said.
He said some of the organisation’s programmes designed to prevent malnutrition and relapse included the social behavioural change programme, which addresses the use of preventive feeding, teaching mothers how to prepare nutritious meals like tombrown, and counselling them on maternal and infant/young child feeding practices, including breastfeeding.
Dr Ojetola, the IMC nutrition coordinator said, “At policy level, I call on the government to ensure integration of Food Security and Livelihood (FSL) and WASH programmes into the existing health structure to ensure that in every nook and cranny, the rate of food insecurity is reduced. This is because all these programmes are interlinked and they all contribute to the success of the child’s health management.”
Olive Muthamia of the Save the Children International, Borno State, said the main way of preventing relapse in children under five was to look at resilience projects by improving the food security of people in the communities, and also by integrating nutrition interventions with other interventions.
Seeking health care on time reduces the chances of relapse, according to Joshua Ayuba Mpato, health promoter and IEC manager, MSF-Belgium in Maiduguri.
He said working on people’s health seeking behaviour helped reduced the relapse rate in the facility.
He said the facility also engaged in home visits, particularly for TB, HIV and sickle cell anemia patients because more relapse cases were seen amongst them.
“We also follow up on the patients after discharge to ensure they are taking the plumpy nuts afterwards,” he said.
During a recent visit to Borno State, it was found that some women sold the plumpy nuts given to their malnourished children.
To get more plumpy nuts to sell, they register their malnourished children in different treatment centres under different names.
Findings showed that the Kasuwan Shanu junction and Kasuwan Biladiwu at Custom roundabout, Maiduguri are popular places for buying and selling diverted plumpy nuts.
A nurse at a treatment centre in Ngomari in Maiduguri who spoke on condition of anonymity said the facility had developed a tracking system that includes asking mothers to keep the children in the centre for staff to administer the plumpy nuts.
“Whenever I receive the RUTF for my child, I share it into two and sell the other half. I give the remaining half to my child because of poverty. I use the money I get from selling it to feed myself, my husband and my other children. If I have a source of livelihood, I would stop selling the RUTF,” said Saadatu Mohammed, a displaced mother of nine children from Baga.
Fatima, a widow, has a daughter who has been treated of acute malnutrition several times. She said, “When I go back to the treatment centre and I am given RUTF, I will still sell part of it to raise money for other pressing needs. I have no alternative source of income to feed my other children,” she said.
A leader of the RUTF retailers at the Kasuwan Shanu junction said health workers usually gave the mothers 18 pieces of RUTF. Then they would sell eight to retailers and go home with the remaining 10 for their babies.
According to her, men who buy the RUTF from them eat it with bread.
This story was supported by the Global Nutrition and Food Security Reporting Fellowship of the International Centre for Journalists (ICFJ) and the Eleanor Crook Foundation.
 Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.
Join Daily Trust WhatsApp Community For Quick Access To News and Happenings Around You.